THE LIVER
Where to Find Your Liver
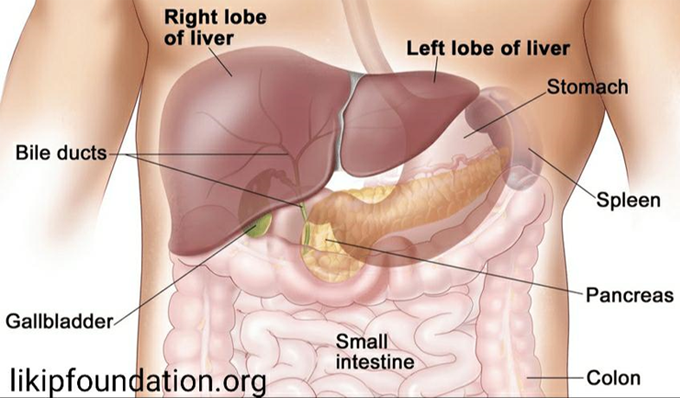
The liver is your body’s largest internal organ, weighing between 3 and 5 pounds. Your liver is located on the right side of your upper body, below the lungs, taking up most of the space in your rib cage. The gallbladder, which stores bile made in the liver, is found tucked under your liver. Your liver is made up of two separate sections, or lobes: the larger right lobe and the smaller left lobe. These two lobes are separated by tissue which anchors your liver in place.
What Your Liver Does
Your liver’s biggest role is to filter your blood all day, every day. A healthy liver gets its color, a deep reddish brown, because it is so drenched in blood. At any given moment, your liver contains about a pint of blood, or 13% of the body’s total blood supply. Your liver filters more than a liter of blood every minute which is about 22 gallons of blood per hour and more than 250 gallons of blood in a 24-hour time period. There are two sources that supply your liver with all that blood: the hepatic
artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood to your liver. Blood coming from your digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
The Parts of Your Liver
As was mentioned earlier, the liver has two lobes. Each lobe is made up of smaller sections called lobules which are clusters of liver cells. The portal vein and the hepatic artery enter the liver sending one large trunk to the left lobe and one large trunk to the right lobe, gradually dividing into smaller branches creating a network of vessels bringing blood to each lobule. Once the cells in the lobule process the blood, ducts (small tubes) transport bile from the cell while filtered blood empties into veins at the center of each lobule. Veins lead out of the lobules merging into larger veins eventually flowing into the hepatic veins; blood then leaves the liver through the inferior vena cava, the largest vein in the body. Ducts transport bile out of the lobule flowing into larger right and left hepatic ducts. These two larger ducts come together to form the common hepatic duct. The common hepatic duct drains the bile to the gallbladder where it is stored and brings bile to the first part of the small intestine.

How Your Liver Works
Unlike the lungs or heart, we cannot feel
our liver working. Many people don’t think about their liver unless or until there is something wrong with it. Your liver is an incredibly hard-working organ with more than 500 different vital functions. Only your brain has more functions than the liver. Many of the liver’s functions are related to your metabolism. These metabolic functions allow you to convert food to energy, break down food to basic building blocks needed by your body and eliminate waste.
The liver…
Produces bile
Bile is a yellow-green acidic liquid that helps carry away waste and break down fats in the small intestine during digestion
Produces proteins for blood plasma
Blood plasma is a fluid which transports blood components (red and white blood cells and platelets), nutrients, hormones, proteins, and waste products
Produces cholesteroland special proteins to help carry fats through the body
Converts unused glucoseinto glycogen for storage
When needed, glycogen can be converted back to glucose for energy
Balances blood sugar and makesglucose as needed
Regulates levels of amino acidsin blood
Amino acids form the building blocks of proteins
Stores iron processed from hemoglobin
Hemoglobin is the protein in your red blood cells that carries oxygen
Converts poisonous ammonia, made during digestion, to urea
Processes drugs and other poisonous substances to your body
Regulates blood clotting (or our ability to stop bleeding)
Fights infections by making immune factors and removing bacteria from the bloodstream
Removes bilirubinfrom red blood cellsThe liver removes harmful substances from our body often by breaking them down to smaller byproducts. These byproducts leave the liver through bile or blood – byproducts in bile are removed from the body through feces while those in the blood are filtered out by the kidneys and removed through urine. This is why Hepatitis or liver disease can devastate a person’s health.
HEPATITIS
What is the meaning of hepatitis?
HEPATITIS Is a combination of two words “HEPA” and “TITIS”. It is derived from the Greek word hêpar (ἧπαρ), meaning “liver”, and -itis (-ῖτις), meaning “inflammation”.
So Hepatitis simply means Inflammation (swelling) of the liver. It is usually the first stage of liver disease. Inflammation is generally a sign that the body is trying to fight an infection or heal an injury. When liver disease is present, inflammation continues over time. This leads to scarring of the liver. Many people with hepatitis have no symptoms; however, some may feel tired or have abdominal (belly area) discomfort. others develop yellow discoloration of the skin and eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Hepatitis is often diagnosed through blood and imaging tests. If the liver disease is diagnosed and treated successfully at this stage, the inflammation may go away. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.
CAUSES OF HEPATITIS
What causes Hepatitis?
The 8 major causes include (1) heavy alcohol use, (2) toxins and chemicals, (3) medications, (4) Food and drinks
(5) sedentary lifestyle and Bad eating habits, (6) autoimmune diseases, (7) genetic factors and (8) Infections (bacterial , parasites, viral)
(1) EXCESSIVE ALCOHOL INTAKE (ALCOHOLIC HEPATITIS)
What is Alcoholic Hepatitis?
Excessive alcohol consumption is a significant cause of hepatitis and is the most common cause of liver cirrhosis. Alcoholic hepatitis is caused by drinking too much alcohol. The liver breaks down alcohol and When alcohol gets processed in the liver, it produces highly toxic chemicals. These chemicals can injure the liver cells. if, over time, you drink more alcohol than the liver can process, it can become seriously damaged. This ranges in order of severity and reversibility from alcoholic steatosis (least severe, most reversible), alcoholic hepatitis, cirrhosis, and liver cancer (most severe, least reversible). Alcoholic hepatitis usually develops over years-long exposure to alcohol, occurring in 10 to 20% of alcoholics. The most important risk factors for the development of alcoholic hepatitis are quantity and duration of alcohol intake. Long-term alcohol intake in excess of 80 grams of alcohol a day in men and 40 grams a day in women is associated with development of alcoholic hepatitis (1 beer or 4 ounces of wine is equivalent to 12g of alcohol). Alcoholic hepatitis can vary from asymptomatic hepatomegaly (enlarged liver) to symptoms of acute or chronic hepatitis to liver failure.
What are possible risk factors for alcoholic hepatitis?
Risk factors include:
- having genetic factors that affect how the body processes alcohol
- living with liver infections or other liver disorders, such as hepatitis B, hepatitis C, and hemochromatosis
- malnutrition
- having a higher body weight
- timing of drinking in relation to eating (drinking during mealtimes lowers the risk of developing alcoholic hepatitis)
What are the symptoms of alcoholic hepatitis?
The following are the most common symptoms of alcoholic hepatitis:
- Belly (abdomen) tenderness or pain over the liver
- Nausea
- Vomiting blood or material that looks like coffee grounds
- Poor appetite
- Yellowing of the skin and eyes (jaundice)
- Weight loss
- Tiredness and weakness
- Fever
- Hepatomegaly
- Fatty liver
Alcoholic hepatitis usually develops over time with continued drinking. But severe alcoholic hepatitis can develop suddenly. It can quickly lead to liver failure and death.
The symptoms of alcoholic hepatitis may look like other health conditions or problems. Always see a doctor for a diagnosis.
What are the complications of alcoholic hepatitis?
Many people with alcoholic hepatitis are infected with the hepatitis C virus, and many have gallstones. They are also at increased risk for liver cancer. If you continue to drink alcohol, the liver will continue to be damaged. Over time, cirrhosis will develop.
Complications of alcoholic hepatitis, which result from severe liver damage, relate to scar tissue. Scar tissue can slow blood flow through your liver, increasing pressure in a major blood vessel (portal vein), and the buildup of toxins. Complications include:
- Enlarged veins (varices).Blood that can’t flow freely through the portal vein can back up into other blood vessels in the stomach and esophagus. These blood vessels have thin walls and are likely to bleed if filled with too much blood. Heavy bleeding in the upper stomach or esophagus is life-threatening and requires immediate medical care.
- Fluid that accumulates in the abdomen might become infected and require treatment with antibiotics. Ascites isn’t life-threatening but are usually a sign of advanced alcoholic hepatitis or cirrhosis.
- Confusion, drowsiness and slurred speech (hepatic encephalopathy).A damaged liver has trouble removing toxins from your body. The buildup of toxins can damage your brain. Severe hepatic encephalopathy can result in coma.
- Kidney failure.A damaged liver can affect blood flow to the kidneys, resulting in damage to those organs.
- This scarring of the liver can lead to liver failure.
How can I prevent Alcoholic Hepatitis?
You might reduce your risk of alcoholic hepatitis if you:
- Drink alcohol in moderation, if at all.For healthy adults, moderate drinking means up to one drink a day for women of all ages and men older than 65, and up to two drinks a day for men age 65 and younger. The only certain way to prevent alcoholic hepatitis is to avoid all alcohol.
- Protect yourself from hepatitis B and C.Hepatitis B and C are infectious liver diseases caused by a viruses. If Untreated, it can lead to cirrhosis. If you have hepatitis B or C and drink alcohol, you’re far more likely to develop cirrhosis than if you didn’t drink.
- Check before mixing medications and alcohol.Ask your doctor if it’s safe to drink alcohol when taking your prescription medications. Read the warning labels on over-the-counter medications. Don’t drink alcohol when taking medications that warn of complications when combined with alcohol — especially pain relievers such as acetaminophen (Tylenol, others).
(2) Toxins or Toxic Hepatitis
What is Toxic Hepatitis?
Toxic hepatitis is the inflammation (swelling) of the liver caused by exposure to toxins from expired foods, adulterated foods, expired drinks, expired drugs or drug over dose and chemicals from the environment. Exposure to toxic chemicals in the workplace, such as dry cleaning solvent carbon tetrachloride, a substance called vinyl chloride (used to make plastics), the herbicide paraquat and a group of industrial chemicals called polychlorinated biphenyls are common cause of toxic hepatitis. Chemicals can enter the environment from many different sources such as landfills, incinerators, tanks, drums, or factories. Cars, trucks, and buses emit exhaust gases while in operation. Industrial and manufacturing processes create solid and hazardous waste. Some wastes contain chemicals that are hazardous to people and the environment. Exposure can occur through ingesting a chemical, breathing it in, or through contact with the skin. Some of these Chemicals include The WHO list of 10 chemicals of public health concern:
- Air pollution
- Arsenic
- Asbestos
- Benzene
- Cadmium
- Dioxins and dioxin-like substances
- Inadequate or excess fluoride
- Lead
- Mercury
- Highly Hazardous Pesticides
Other source of harmful toxic exposure is tobacco Smoking.
SMOKING
Direct smoking and second hand smoking can increase the risk of both liver cancer and cirrhosis of the liver. The toxic chemicals in tobacco smoke can cause inflammation and eventual cirrhosis. Smoking also promotes the production of cytokines, chemicals that cause even more inflammation and damage to liver cells. Another concern: In people with hepatitis B or C, smoking can increase the risk of hepatocellular carcinoma, a form of liver cancer.
Is Secondhand Smoke as Dangerous as Smoking a Cigarette?
Secondhand smoke refers to the fumes that are emitted when smokers use:
- cigarettes
- pipes
- cigars
- other tobacco products
Firsthand smoking and secondhand smoke both cause serious health effects. While directly smoking is worse, the two have similar adverse health effects.
Secondhand smoke is also called:
- side-stream smoke
- environmental smoke
- passive smoke
- involuntary smoke
Nonsmokers who inhale secondhand smoke are affected by chemicals contained in the smoke.
According to the WHO, there are over 7,000 chemicals found in tobacco smoke. In all, at least 69 are cancerous. Over 250 are harmful in other ways.
Fluids such as blood and urine in nonsmokers might test positive for nicotine, carbon monoxide, and formaldehyde. The longer you’re exposed to secondhand smoke, the greater the risk you are of inhaling these toxic chemicals.
Exposure to secondhand smoke occurs anywhere someone might be smoking. These places can include:
- bars
- cars
- homes
- parties
- recreational areas
- restaurants
- workplaces
Overall, WHO estimates that 1.2 million premature deaths per year are related to secondhand smoke worldwide.
This is a serious health concern that can affect both adults and children who are exposed to secondhand smoke.
The only way to eliminate such risks is to stay away from tobacco smoke entirely.
How does secondhand smoke affect nonsmokers?
Secondhand smoke damages the body in many different ways. Adults exposed to secondhand smoke may experience:
- Cardiovascular (heart, veins and arteries) disease like high blood pressure, atherosclerosis, heart attack or stroke.
- Lung problems like chronic obstructive pulmonary disorder (COPD) and asthma.
- Increased risks of lung cancer and cancers in the brain, bladder, stomach, breast and more.
- Children exposed to secondhand smoke are more likely to experience:
- Frequent coughing, sneezing, shortness of breath or other breathing problems.
- Frequent ear infections.
- Fatty liver Disease
- Frequent and more severe asthma attacks.
- Respiratory infections, such as bronchitis or pneumonia.
- Damage to eyes (like cataracts) and teeth (like tooth decay).
- Learning and behavior problems.
- SIDS (sudden infant death syndrome).
When does secondhand smoke damage start?
Studies have shown that damage from secondhand smoke occurs in as little as five minutes:
- After five minutes: Arteries becomes less flexible, just like they do in a person who is smoking a cigarette.
- After 20-30 minutes: Blood starts clotting, and fat deposits in blood vessels increase the risk of heart attack and stroke.
- After two hours: An irregular heartbeat (arrhythmia) can develop and trigger a heart attack or other serious cardiac problems.
Can inhalation of secondhand smoke be treated?
There is no treatment for breathing in secondhand smoke. But there are ways to manage your exposure and treat conditions related to secondhand smoke inhalation.
If you are regularly near secondhand smoke, you can reduce the danger by:
- Moving away from the smoker and finding a smoke-free place.
- Making sure guests to your home know they cannot smoke inside.
- Not letting passengers smoke in your car — even with the window down.
Your healthcare provider may treat specific symptoms or diseases caused by secondhand smoke exposure. For example, you may need medications to manage high blood pressure or inhalers to treat asthma or COPD.
MEDICATIONS/ DRUGS
What is drug-induced hepatitis?
Drug-induced hepatitis is a redness and swelling (inflammation) of the liver that is caused by a harmful (toxic) amount of certain medicines. The liver helps to break down certain medicines in your blood. If there is too much medicine in your blood for your liver to break down, your liver can become badly damaged. This can lead to drug-induced hepatitis. It is caused when you have a harmful or toxic amount of some medicines, vitamins, herbal remedies, or food supplements. In most cases, you may be taking a medicine for several months before it reaches a toxic level and affects your liver. This is especially true if you take multiple medications or take more than the recommended dose of medication. But the disease can also happen if you take too much of some medicines, such as acetaminophen. In this case, it can happen quickly. Other times it is an allergic reaction. When a person has an allergic reaction to a drug, liver inflammation occurs due to the immune system’s attempts at fighting back the drugs. Medications come in various forms such as Tablets, Capsules, Liquid, Topical (creams, lotions, ointment), Suppositories, Drops (eye, ear, nose), Inhalers, Injections, Implants, Skin Patches etc.These medications include prescription medications, Over-the-counter (OTC) drugs, herbal and dietary supplements. Many types of drugs can cause liver injury, including :
*PAIN KILLERS such as paracetamol, ibuprofen, diclofenac, aspirin and naproxen .
*ANTIBIOTICS such as isoniazid, nitrofurantoin, amoxicillin-clavulanate(Augmentin), erythromycin, and trimethoprim-sulfamethoxazole;
*ANTICONVULSANTS such as valproate and phenytoin;
*CHOLESTEROL-LOWERING such as
- Atorvastatin (Lipitor)
- Lovastatin (Altoprev)
- Pitavastatin (Livalo, Zypitamag)
- Pravastatin (Pravachol)
- Rosuvastatin (Crestor, Ezallor)
- Simvastatin (Zocor)
*STEROIDS such as oral contraceptives and anabolic steroids (man-made medicines that are like the male sex hormone testosterone ); and
* ANTI-RETROVIRAL therapy used in the treatment of HIV/AIDS. Of these, amoxicillin-clavulanate (Augmentin) is the most common cause of drug-induced liver injury, and paracetamol toxicity is the most common cause of acute liver failure in the United States and Europe.
Herbs and supplements. herbal and dietary supplements, can also cause hepatitis. Some herbs considered dangerous to the liver include aloe vera, black cohosh, cascara, chaparral, aloe vera, saw palmetto, Germander, Pennyroyal, comfrey, kava, ephedra and some dietary supplements marketed for weight loss, bodybuilding, or improvements in sexual function, general well-being, or mental acuity.
There are many others. Children can also develop liver damage if they mistake vitamin supplements for candy and take large doses. Keep in mind that not all “natural” or “herbal” supplements are safe. Taking an expired drug can also increase your risk of hepatitis. Many medications can damage your liver, especially if taken frequently or combined with alcohol.
DRUG ABUSE:The use of illegal drugs or the use of prescription or over-the-counter drugs for purposes other than those for which they are meant to be used, or in excessive amounts can also damage your liver.
Prescription/medication Errors.
A medication error is defined as “any preventable event that may cause or lead
to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer,”
Medication errors can occur throughout the medication-use system. Such as, when prescribing a drug, upon entering information into a computer system, when the drug is being prepared or dispensed, or when the drug is given to or taken by a patient. So Doctors, nurses, pharmacists or Medicine Counter Assistants, care givers and patients are all involved.
Medication errors refer to mistakes in prescribing, dispensing and giving medications. They injure hundreds of thousands of people every year in the United States. Yet most medication errors can be prevented. How can you protect yourself and your family?
One of the best ways to reduce your risk of a medication error is to take an active role in your own health care. Learn about the medications you take — including possible side effects. Never hesitate to ask questions or share concerns with your doctor, pharmacist and other health care providers.
What exactly are medication errors?
Medication errors are preventable events due to the inappropriate use of medications. Medication errors that cause harm are called preventable adverse drug events. If a medication error occurred, but didn’t hurt anyone, it’s called a potential adverse drug event. An example of a medication error is taking an over-the-counter product that contains acetaminophen (Tylenol, others) when you’re already taking a prescription pain medicine that contains this exact ingredient. This mistake could cause you to take more than the recommended dose of acetaminophen, putting yourself at risk of liver damage.
Another example of a possible medication error is taking a depression medication called fluoxetine (Prozac, Sarafem) with a migraine drug called sumatriptan (Imitrex). Both medicines affect levels of a brain chemical called serotonin. Taking them together may lead to a potentially life-threatening condition called serotonin syndrome. Symptoms of the dangerous drug interaction include confusion, agitation, rapid heartbeat and increased
body temperature, among others.
How do medication errors happen?
Medication errors can happen to anyone in any place, including your own home and at the doctor’s office, hospital, pharmacy and senior living facility. Kids are especially at high risk for medication errors because they typically need different drug doses than adults.
Knowing what you’re up against can help you play it safe. The most common causes of medication errors are:
- Poor communication between your doctors
- Poor communication between you and your doctors
- Drug names that sound alike and medications that look alike
- Medical abbreviations
- Patient names that look alike
- Unclear hand writing from Doctors
Know how to prevent medication errors
Knowledge is your best defense. If you don’t understand something your doctor says, ask for an explanation. Whenever you start a new medication, make sure you know the answers to these questions:
- What is the brand or generic name of the medication?
- What is the medication supposed to do? How long will it be until I see results?
- What is the dose? How long should I take it?
- What should I do if I miss a dose?
- What should I do if I accidentally take more than the recommended dose?
- Are there any foods, drinks, other medications or activities I should avoid while taking this medicine?
- What are the possible side effects? What should I do if they occur?
- Will this new medication interfere with my other medication(s)? If so, how?
Your doctor can help prevent medication errors by using a computer to enter and print (or digitally send) any prescription details, instead of hand writing one.
Participate in medication reconciliation
Asking questions is essential, but it isn’t enough. Your Doctor can follow a process called medication reconciliation to significantly decrease your risk of medication errors.
Medication reconciliation is a safety strategy that involves comparing the list of medications your Doctor currently has with the list of medications you are currently taking. This process is done to avoid medication errors such as:
- Missing medications (omissions)
- Duplicate medications
- Dosing errors
- Drug interactions
Medication reconciliation should be done at every transition of care in which new medications are ordered or existing orders are rewritten. Transitions in care include changes in setting (such as being admitted or discharged from the hospital), health care provider or level of care.
Sharing your most up-to-date information with your health care providers gives the
clearest picture of your condition and helps avoid medication mistakes.
Here’s what you need to tell your health care providers:
- The name and strength of all medications you’re taking and when you take them, including prescription medications, herbs, vitamins, nutritional supplements, over-the-counter drugs, vaccines and anything received intravenously, including diagnostic and contrast agents, radioactive medications, feeding tube supplements and blood products
Any medications that you’re allergic to or that have caused problems for you in the past
- Whether you have any chronic or serious health problems
- If you might be pregnant or you’re trying to become pregnant
Avoid these mistakes
The following medication errors have happened to some people. Don’t make these same mistakes:
- Confusing eardrops and eyedrops.Always double-check the label. If a medication says “otic,” it’s for the ears. If it says “ophthalmic,” it’s for the eyes.
- Chewing nonchewables.Don’t assume chewing a pill is as good as swallowing it. Some medications should never be chewed, cut or crushed. Doing so may change how they’re absorbed by the body.
- Cutting up pills.Never split pills unless your doctor or pharmacist has told you it’s safe to do so. Some medications shouldn’t be cut because they’re specially coated to be long acting or to protect the stomach.
- Using the wrong spoon.The spoons in your silverware drawer aren’t measuring spoons. To get an accurate dose, use an oral syringe (available at pharmacies) or the dose cup that came with the medication.
Make safety a habit
Get into the habit of playing it safe with these medication tips:
- Keep an up-to-date list of all your medications, including nonprescription drugs and supplements.
- Store medications in their original labeled containers.
- Keep your medications organized by using a pillbox or an automatic pill dispenser.
- Save the information sheets that come with your medications.
Use the same pharmacy, if possible, for all of your prescriptions.
- When you pick up a prescription, check that it’s the one your doctor ordered.
- Don’t give your prescription medication to someone else and don’t take someone else’s.
A final word on medication errors
“Don’t ask, don’t tell” is never a smart policy when it comes to medications and your health. Don’t hesitate to ask questions or to tell your health care providers if anything seems amiss. Remember, you’re the final line of defense against medication errors.
FOOD AND DRINKS
Some food packages and cookware can leak toxins into your food. Some food and drinks contains additives and preservatives that can be harmful when taken in large amounts. Also, consuming expired food or drink can increase your risk of liver injury. Some foods have also been poisoned with adulterants. For example.
AUGUST 2008 RESEARCH
“A survey conducted by Food and Drugs Board and the Food Research Institute (FRI) of the Council for Scientific and Industrial Research (CSIR) showed that various substances were added to various foods by those who prepared them and warned that this was an offence and liable to imprisonment. Mrs.
Isabella Mansa Agra, Head of Food Registration and Nutrition of the FDB, in a document copied to the Ghana News Agency, said food adulteration is on the increase and common in Ghanaian urban markets with the perpetrators playing on the ignorance of innocent buyers.
She said the survey revealed that alum and chalk were added to bread to whiten it, while for stale flour, ammonium carbonate was added to disguise its sour taste.
Mashed potatoes, sawdust and Plaster of Paris were also added to increase the weight of the bread. Mrs Agra noted that food dyes, colours and miscellaneous compounds were added to food to impart certain properties to disguise deteriorated or spoiled food and give an idea of freshness. The study, conducted in eight regions, sought to provide some leads for the relevant authorities to work with.
It indicated that saccharine was also added to maize porridge, sugar bread and doughnuts to sweeten the taste of the products whilst cassava flour, roasted maize meal, maize flour, dried, grinded pear seed, cooking oil, water and fresh cassava chips were added to groundnut paste to increase its weight.
The regions selected for the study were Greater Accra, Volta, Eastern, Central, Brong Ahafo Western, Northern and Ashanti. Food adulteration is an act of adding or mixing something inferior, harmful, useless and unnecessary to food.
It is intended to reduce manufacturing cost, increase bulk or weight, make it appear better and conceal inferiority. Mrs Agra noted that maize flour, milled fresh groundnuts, gari and wheat flour were added to grinded agushie to increase its weight and this act was common in Eastern, Northern, Western, Central and Greater Accra regions.
For fruits and vegetables, bixa, pear seeds and discarded kola nuts were found in ground pepper and fresh tomatoes before it is grinded whilst wood ash was also found in dried okro powder.
Meat, poultry, fish and shrimps were not out. Bixa seeds are also used for grilled meat popularly known as khebab and fried turkey tails and these were common in the Central and Greater Accra regions. For fat and oils like palm oil, dzomi, coconut oil, groundnut oil and soyabean oil; palm kernel oils, Sudan Dyes, were added and these were found in Greater Accra, Volta, Eastern, Ashanti, Central and Western regions.
“It is also shocking to know that beverages like palm wine and pito are also adulterated and surprisingly, for palm wine, water, sugar, saccharine, miracle berry monosodium glutamate, baking soda and tobacco leaves were added to sweeten them.”
Tobacco leaves and marijuana were also found in pito to enhance its stimulant effects.
For miscellaneous foods, sugar, honey, baking powder, curry powder, soups and stews, water, caramel, wheat flour, granulated salt, maize flour and bixa seeds were added to enhance their sweetness.
Mrs Agra explained that the adulterants such as saccharine and aspartame could cause cancer whilst monosodium glutamate used in soups, stews and meat could damage the brain, cause mental retardation in infants and other food flavours also had the chance of causing cancer of the liver.
Cola nuts, cassava flour and Sudan dyes used in pepper, groundnut paste and palm oil could increase anxiety and nervousness at high doses, decrease nutritive value of products and cause cancer.
“Potassium bromate (E924) used in bread has the chance of causing cancer and nitrate used in tendering meat and beans could cause cancer and tumours in the liver, kidney, trachea oesophagus and lungs,” she added.
Mrs Agra cautioned that the Food and Drugs law prohibited the sale of unwholesome, poisonous or adulterated food and any person found violating the law would be punished.” -www.modernghana.com
May 2015 Research
“The Food and Drugs Authority (FDA) has cautioned against the mixing of food with adulterants, describing it as injurious to human health.
It said food adulteration was on the increase and very common on the Ghanaian urban markets with perpetrators plying on the ignorance of innocent buyers.
He, therefore, urged consumers to report any unusual changes in their food to the FDA.
Mr Edward Archer, a Principal Regulator of the Food Safety Management Unit of the FDA, gave the caution at a Food Safety Advocacy Campaign for Traditional Caterers Association members in Greater Accra.
Mr Acher defined food adulteration is an act of adding or mixing something inferior, harmful, useless and unnecessary to food.
It is intended to reduce manufacturing cost, increase bulk or weight, to make it appear better and conceal inferiority.
The seminar was organized with the Queen Mothers? Foundation of Ghana to raise the awareness of caterers on the dangers associated with food adulteration and the need to be on the lookout and help in the campaign against it.
Mr Acher pointed out that even colours used in making tie and dyes designs, and miscellaneous compounds were mixed with some foods to impart certain properties and to disguise deteriorated or spoiled foods to give an idea of freshness.
He said cassava flour, roasted maize meal, maize flour, dried and grinded pear seed, cooking oil, water and fresh cassava chips were also added to groundnut paste to increase its weight.
Maize flour, milled fresh groundnuts, gari and wheat flour, he said, were also added to grinded agushie to increase its weight.
?This act is very common, thus posing so much danger to consumers? health,? he complained.
For fat and oils like palm oil, dzomi, coconut oil, groundnut oil and soyabean oil; palm kernel oils, he said, Sudan Dyes, were added to give it the red colour, which he said, was the demand of consumers.
He explained that cola nuts and Sudan dyes used in pepper, groundnut paste and palm oil could increase anxiety and nervousness at high doses, decrease nutritive value of products and could even cause cancer.
Mr Acher urged the caterers and the public to report any unusual change in the food items they buy from the market to FDA for the necessary actions to be taken.
Ms Maria Lovelace-Johnson, the Head of the Food Safety Management Unit of the FDA, took participants through the five keys to keep their food safe.
The five keys, she explained, were keeping themselves clean, separating raw food from cooked food, cooking and reheating their food well to avoid contamination, keeping food at safe temperatures and always using wholesome raw materials and buying from clean places.
She noted that if these steps were not taken, it could lead to food poisoning and reiterated the the Food and Drugs Law prohibited the sale of unwholesome, poisonous or adulterated for foods.
Members of the Foundation said they were ready to prevent food-borne illness, hence, the initiative to collaborate with FDA to educate women.” -www.newsghana.com
December 2020 Research
“Food fraud in Ghana
Food fraud strategies in Ghana include adulteration, substitution and counterfeiting of
food products. A common practice is the adulteration and substitution of products with
similar ones of low quality, either partially or completely, which eventually expose
consumers to health risks and allergic complications.
For instance, palm oil, a major locally produced food product, has been found to be
adulterated with Sudan dyes (I, II, III and IV). Other products that have been found to be
adulterated or substituted with harmful substances include honey products, alcohol, palm
wine, and cheese.
It was reported in 2019 that organochemicals with lindanes and endosulfans were the
most abundant agro-based insecticide residues found in vegetables and some fruits in
the country (2). Similar findings were presented by Gonu et al. (3) in sampled fruit-based
drinks in the capital city of Ghana, which even though were below the EUs MRLs, the
levels detected significantly affect the wholesomeness of the products.
A 2011 research by Tutu et al. (4) showed high levels of organochlorine pesticide
residues in the breast milk of primiparae mothers in La, a suburb of Accra. This was after
numerous scientific studies indicated that common items on the local market such as
powdered pepper, groundnut paste, fish and tomatoes powder contained chuff,
condiments and unknown amounts of foreign materials.
Although this situation is being tackled by national institutions, such as the Food & Drugs
Authority (FDA), news headlines about the identification of fake food products show how
the fight against food fraud in Ghana require more efforts than just normal conventional
investigative methods.”
-www.resarchgate.net
(5) SEDENTARY LIFESTYLE AND BAD EATING HABITS
What is an inactive or sedentary lifestyle?
Not exercising. A sedentary or inactive lifestyle. You have probably heard of all of these phrases, and they mean the same thing: a lifestyle with a lot of sitting and lying down, with very little to no exercise.
Around the world, people are spending more and more time doing sedentary activities. During our leisure time, we are often sitting: while using a computer or other device, watching TV, or playing video games. Many of our jobs have become more sedentary, with long days sitting at a desk. And the way most of us get around involves sitting – in cars, on buses, and on trains.
How does an inactive lifestyle affect your body?
When you have an inactive lifestyle,:
- You burn fewer calories. This makes you more likely to gain weight.
- You may lose muscle strength and endurance, because you are not using your muscles as much
- Your bones may get weaker and lose some mineral content
- Your metabolism may be affected, and your body may have more trouble breaking down fats and sugars
- Your immune system may not work as well
- You may have poorer blood circulation
- Your body may have more inflammation
- You may develop a hormonal imbalance
What are the health risks of an inactive lifestyle?
Having an inactive lifestyle can be one of the causes of many chronic diseases. By not getting regular exercise, you raise your risk of:
- Obesity
- Heart diseases, including coronary artery disease and heart attack
- High blood pressure
- High cholesterol
- Stroke
- Metabolic syndrome
- Type 2 diabetes
- Certain cancers, including colon, breast, and uterine cancers
- Osteoporosis and falls
- Increased feelings of depression and anxiety
- Non Alcoholic Fatty Liver Disease
Having a sedentary lifestyle can also raise your risk of premature death. And the more sedentary you are, the higher your health risks are.
How can I get started with exercise?
If you have been inactive, you may need to start slowly. You can keep adding more exercise gradually. The more you can do, the better. But try not to feel overwhelmed, and do what you can. Getting some exercise is always better than getting none. Eventually, your goal can be to get the recommended amount of exercise for your age and health.
There are many different ways to get exercise; it is important to find the types that are best for you. You can also try to add activity to your life in smaller ways, such as at home and at work.
How can I be more active around the house?
There are some ways you can be active around your house:
- Housework, gardening, and yard work are all physical work. To increase the intensity, you could try doing them at a more vigorous pace.
- Keep moving while you watch TV. Lift hand weights, do some gentle yoga stretches, or pedal an exercise bike. Instead of using the TV remote, get up and change the channels yourself.
- Work out at home with a workout video (on your TV or on the internet)
- Go for a walk in your neighborhood. It can be more fun if you walk your dog, walk your kids to school, or walk with a friend.
- Stand up when talking on the phone
- Get some exercise equipment for your home. Treadmills and elliptical trainers are great, but not everyone has the money or space for one. Less expensive equipment such as yoga balls, exercise mats, stretch bands, and hand weights can help you get a workout at home too.
How can I be more active at work?
Most of us sit when we are working, often in front of a computer. In fact, It can be challenging to fit physical activity into your busy workday, but here are some tips to help you get moving:
- Get up from your chair and move around at least once an hour
- Stand when you are talking on the phone
- Find out whether your company can get you a stand-up or treadmill desk
- Take the stairs instead of the elevator
- Use your break or part of your lunch hour to walk around the building
- Stand up and walk to a colleague’s office instead of sending an email
- Have “walking” or standing meetings with co-workers instead of sitting in a conference room
BAD EATING HABITS

Healthy diet and habits help maintain the proper functioning of the organs in your body. A poor diet and sedentary lifestyle will impact a person’s overall health and contribute to dysfunction or deterioration of vital organs, including the liver.
When you eat food, it is broken down in your stomach and intestine (gut) and three main nutrients are extracted:
- carbohydrates
- fat
- protein
These nutrients are then absorbed into the bloodstream and carried to your liver. Here they are either stored, or changed in such a way that your body can use them at once.
Some liver diseases are linked to build up of fat in the liver. This leads to a condition called non-alcohol related fatty liver disease (NAFLD). If fatty deposits build up over a long time they can damage the liver and stop it working properly. People are more likely to develop NAFLD if they have an unhealthy diet or they live with overweight or obesity.
Obesity can also speed the damage associated with other conditions such as alcoholic liver disease and can decrease the effectiveness of treatments for hepatitis C .
It is important to maintain a healthy weight. To do this you need to balance the amount of food you eat with the energy you need. If you eat more than you use, your weight will increase. If you eat fewer calories than your body uses you will lose weight. There are two ways to shift the balance of calories and lose weight. Eat a healthy, balanced diet. And be more physically active. Correct the habit of late night Eating.
Sugar
Too much sugar isn’t just bad for your teeth. It can harm your liver, too. The organ uses one type of sugar, called fructose, to make fat. Too much refined sugar and high-fructose corn syrup causes a fatty buildup that can lead to liver disease. Some studies show that sugar can be as damaging to the liver as alcohol, even if you’re not overweight. It’s one more reason to limit foods with added sugars, such as soda, pastries, and candy.
Trans Fats
Trans fats are a man-made fat in some packaged foods and baked goods. (You’ll see them listed as “partially hydrogenated” ingredients). A diet high in trans fats makes you more likely to gain weight. That’s not good for your liver. Check the ingredients list. Even if it says “0” grams of trans fat, it may still have a small amount, and that adds up.
Fast food damages the liver
a Swedish study of 34 people that looked at the effects on the liver of a diet high in saturated fat when levels of exercise are kept to a minimum. People who were “fed fast food twice a day for a month began to show signs of liver damage after only a week”, “People who gorged junk food and shunned exercise for four weeks had liver enzyme changes that usually indicate alcohol abuse.”
www.nicswell.co.uk
When you eat may contribute to fatty liver disease as much as what you eat
Recently at the American Association for the Study of Liver Diseases annual meeting, a study was reported that suggested WHEN we eat influences the development of fatty liver disease.
It was found that skipping breakfast and lunch increased the risk of fatty liver disease by 20% and 73% respectively. Eating between 10 PM and 4 AM increased the risk of fatty liver disease by 61%. Eating more of the day’s calories in the morning decreased the risk of fatty liver disease by up to 21%. Researchers adjusted for total calorie intake, age, gender, alcohol use and taking medications that are hard on the liver.
What recommendations can we give people based on this research? These findings really reinforce the common-sense recommendations we give people all the time.
- Eat breakfast every day
- Eat lunch every day
- Don’t eat too close to bedtime
What about shift workers? What about my nurses and others that work the night shift? It doesn’t seem to matter what time you are awake. The liver has its own circadian rhythm and it seems that eating in the middle of the night is bad for your liver no matter when you sleep.
Since we know that night-shift workers are at higher risk for obesity and other health problems than those who work and are active during the day, this may be one way to reduce the health risks associated with night shift work. Keeping the calorie intake mirroring how day-shift workers eat may help to mitigate the risks for night shift workers.
For instance, one could eat a large “breakfast” when coming off-shift, a medium-sized “lunch” prior to sleep, a small “dinner” before heading to work, and avoid eating in the middle of the night while working.
Simple tips to stop late-night cravings
A few basic strategies may help you avoid eating late at night.
- Enjoy regular meals. Eating regular meals throughout the day — especially ones that are very filling, such as those high in fiber and protein — may reduce your desire to eat late at night.
- Avoid keeping snacks at home. “Out of sight, out of mind” pertains to late-night snacking. The more visible a food is, the likelier you are to eat it. If you’re tempted to snack at night, place snacks where you can’t see them — or avoid keeping them at home.
- Brush your teeth. When you brush your teeth, it’s like telling your body that you’re done eating for the day. Plus, some foods don’t taste good after brushing.
- Eat fruits. Instead of rummaging through the fridge after a long day, try forming new healthy habits that don’t involve eating heavy. One simple idea is to take fruits
- Go to sleep early. Staying up late may give you more opportunities to raid the fridge at night. Also, getting insufficient sleep may raise hunger hormone levels, leading you to eat more. Aim for 7–8 hours of sleep each night
(6)AUTOIMMUNE DISEASES
What is autoimmune hepatitis?
Autoimmune hepatitis occurs when your body’s infection-fighting system (immune system) attacks your liver cells. This causes swelling, inflammation and liver damage.
Autoimmune Hepatitis is uncommonMen and women can develop Autoimmune Hepatitis but it is 3 to 4 times more common in women. It can develop at any age, however, it is more commonly diagnosed in women around the age of 45. It can affect all ethnic groups. Thirty to fifty percent of people diagnosed with Autoimmune Hepatitis have another autoimmune condition, such as thyroid disease, rheumatoid arthritis, ulcerative colitis or Type 1 diabetes.
What causes Autoimmune Hepatitis?
The cause of most cases of Autoimmune Hepatitis is not clear; but is thought to be a mixture of:
- autoimmunity – the process of your immune system making autoantibodies, which ‘attack’ and damage your body’s own cells and organs
- environmental triggers – causes starting outside of the body; for example getting a virus, taking certain medications, or coming into contact with other toxins
- genetic predisposition – inheriting genes which may make it easier for a trigger to set off the disease.
(7) GENETIC Or INHERITED LIVER DISEASE
The two most common inherited liver diseases are hemochromatosis and alpha-1 antitrypsin deficiency.
Hemochromatosis
Hemochromatosis is a disease in which deposits of iron collect in the liver and other organs. The primary form of this disease is one of the most common inherited diseases in the U.S. — up to one in every 200 people has the disease, many unknowingly. When one family member has this disorder, siblings, parents, and children are also at risk.
A secondary form of hemochromatosis is not genetic and is caused by other diseases, such as thalassemia, a genetic blood disorder that causes anemia.
The iron overload associated with hemochromatosis affects men more often than it does women. Because women lose blood through menstruation, women are unlikely to show signs of iron overload until after menopause. Hemochromatosis is more common in people of Western European descent.
What Are the Symptoms of Hemochromatosis?
The symptoms of hemochromatosis may include:
- Liver disease
- Joint pain
- Fatigue
- Unexplained weight loss
- A darkening of the skin frequently referred to as “bronzing”
- Abdominal pain
- Loss of sexual desire
People with hemochromatosis may also have signs of diabetes and heart disease and may also develop liver cancer, cirrhosis, testicular atrophy (wasting away), and infertility.
How Is Hemochromatosis Diagnosed and Treated?
Whenever hemochromatosis is suspected, a blood test to look for excess iron in the blood is performed. If excess iron is found, a genetic blood test (hemochromatosis DNA test) may be ordered. The genetic test is also used to screen family members of patients with a positive genetic test. The goal of treatment is to remove excess iron from the body, as well as reduce any symptoms or complications that have resulted from the disease.
Excess iron is removed from the body in a procedure called phlebotomy. During the procedure, one-half liter of blood is removed from the body each week for a period of up to two or three years until the iron buildup has been reduced.
After this initial treatment, phlebotomies are needed less frequently. The frequency varies based on individual circumstances.
Another treatment for hemochromatosis is iron chelation therapy. Iron chelation uses medicine to remove excess iron from your body, and it is a good option for people who can’t have routine blood removal.
Alpha-1 Antitrypsin Deficiency
In this inherited liver disease an important liver protein known as alpha-1 antitrypsin is either lacking or exists in lower than normal levels in the blood. People with alpha-1 antitrypsin deficiency are able to produce this protein; however, the disease prevents it from entering the bloodstream and it instead accumulates in the liver.
Alpha-1 antitrypsin protein protects the lungs from damage due to naturally occurring enzymes. When the protein is too low or non-existent, the lungs can become damaged, leading to difficulty breathing and, in many people with the condition, emphysema. People with this disease are also at risk of developing cirrhosis.
What Are the Symptoms of Alpha-1 Antitrypsin Deficiency?
The first symptoms of alpha-1 antitrypsin deficiency will usually be symptoms of its effects on the lungs, including shortness of breath or wheezing. Unexplained weight loss and a barrel-shaped chest, which is commonly associated with the presence of emphysema, can also be signs of the condition. As the disease progresses, symptoms typical of emphysema or cirrhosis include:
- Fatigue
- Chronic cough
- Swelling of the ankles and feet
- Jaundice (this is more commonly associated with cirrhosis)
- Fluid in the abdomen (ascites)
How Is Alpha-1 Antitrypsin Deficiency Diagnosed and Treated?
Physical signs, such as a barrel-shaped chest and respiratory problems, may lead your doctor to suspect alpha-1 antitrypsin deficiency. A blood test that tests specifically for the alpha-1 antitrypsin protein will help confirm the diagnosis.
There is no established treatment to cure alpha-1 antitrypsin deficiency but it can be treated by replacing the protein in the bloodstream. However, experts are not clear on how effective this technique is and who should receive it. Other approaches to treating alpha-1 antitrypsin deficiency involve treating the complications of emphysema and cirrhosis. This includes antibiotics to combat respiratory infections, inhaled medication to make breathing easier, and diuretics and other medication to reduce any fluid buildup in the abdomen.
Personal behavior, such as avoiding alcohol, quitting smoking, and eating a healthy diet, can also help keep symptoms and complications from becoming severe. Your health care provider or dietitian can recommend a diet that is right for you.
SICKLE CELL HEPATOPATHY
liver complications can occur for people with SCD. They may be due to the disease, to treatments, or both. The term sickle cell hepatopathy describes the overlapping causes of liver disease in people with SCD. Sickle cell disease (SCD) or its treatments cause liver problems for many people. Sickling of blood cells in the liver can block blood flow and cause acute complications. Blood transfusions also increase the risk for liver damage from iron overload and hepatitis.
What causes liver problems In Sickle cell disease ?
The major risk factor is receiving multiple blood transfusions. This is linked to hepatitis infection (rarely) and high iron levels, which can both cause liver damage. However, SCD can cause liver problems in many other ways. Liver problems are most common in people with sickle cell anemia (HbSS).
Sickle cells tend to get stuck in blood vessels and block blood flow. When this happens in the liver, liver cells cannot get enough oxygen. This can cause liver cell death and prevent the liver from working properly.
Sickle cells also burst easily because they are unstable. When they burst, they release hemoglobin into the bloodstream. Hemoglobin gets broken down to a substance called bilirubin. When too many sickle cells burst, too much bilirubin builds up in the body. A high level of bilirubin (hyperbilirubinemia) is very common in people with SCD. This can form gallstones in the gallbladder, which can lead to liver problems. Very high bilirubin levels are seen in people with intrahepatic cholestasis.
(8) PATHOGENIC DISEASES
In biology,a pathogen (Greek: πάθος, pathos “suffering”, “passion” and -γενής, -genēs “producer of”) in the oldest and broadest sense, is any organism that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ. Pathogens are different and can cause disease upon entering the body. All a pathogen needs to thrive and survive is a host. Once the pathogen sets itself up in a host’s body, it manages to avoid the body’s immune responses and uses the body’s resources to replicate before exiting and spreading to a new host.
Pathogens can be transmitted in different ways depending on the type. They can be spread through skin contact, bodily fluids, airborne particles, contact with feces, and touching a surface touched by an infected person.
Pathogen types
There are different types of pathogens, but we’re going to focus on the three most common types: bacteria, parasites and viruses.
Bacteria
Bacteria are microorganisms made of a single cell. They are very diverse, have a variety of shapes and features, and have the ability to live in just about any environment, including in and on your body. Not all bacteria cause infections. Those that can are called pathogenic bacteria. Your body can be more prone to bacterial infections when your immune system is compromised by a virus. The disease state caused by a virus enables normally harmless bacteria to become pathogenic. Antibiotics are used to treat bacterial infections. Some strains of bacteria have become resistant to antibiotics, making them difficult to treat. This can happen naturally, but also happens because of the overuse of antibiotics, according to the World Health Organization (WHO). Typhoid Fever is an example of bacteria infection that can cause Hepatitis.
Typhoid fever continues to be a common infection in the developing countries. William Osler initially reported hepatic involvement of typhoid fever in 1899. Hepatomegaly and moderate elevation of transaminase levels are the common findings that occur in 21–60% of cases of typhoid fever. This condition is called Salmonella Hepatitis.
Parasites
Parasites are organisms that behave like tiny animals, living in or on a host and feeding from or at the expense of the host. Though parasitic infections are more common in tropical and subtropical regions, they can occur anywhere.
Three main types of parasites can cause disease in humans. These include:
- protozoa, which are single-celled organisms that can live and multiply in your body
- helminths, which are larger, multi-celled organisms that can live inside or outside your body and are commonly known as worms
- ectoparasites, which are multi-celled organisms that live on or feed off your skin, including some insects, such as ticks and mosquitos
They can be spread several ways, including through contaminated soil, water, food, and blood, as well as through sexual contact and via insect bites. Malarial and Liver flukes are some examples of a parasitic infections that can cause Hepatitis.
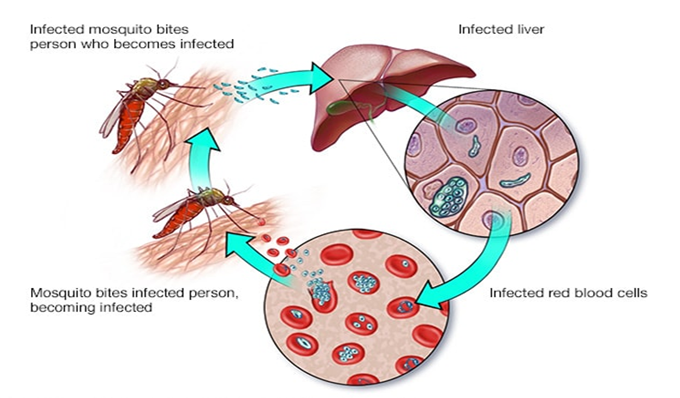
Malarial Hepatitis
When the malaria-causing Plasmodium parasite first slips into the human bloodstream, injected by the bite of an infected mosquito, it does not immediately target red blood cells. Instead, it seeks refuge inside the liver and uses the liver cells to rapidly reproduces, copying itself as many as 30,000 times in the span of 48 hours. After building strength in numbers, the parasite leaves the liver and escapes into the blood stream, invading red blood cells and triggering the devastating disease. Malaria Complications can damage the kidneys or liver or cause the spleen to rupture.
Liver Flukes
A liver fluke is a parasitic worm. Infections in humans usually occur after eating contaminated raw or undercooked vegetables , crab, fish or meat. After liver flukes have been ingested, they travel from your intestines to your bile ducts in your liver where they then live and grow. While most infected persons do not show any symptoms, infections that last a long time can result in severe symptoms and serious illness. Untreated, infections may persist for up to 25–30 years, the lifespan of the parasite. Typical symptoms include indigestion, abdominal pain, diarrhea, or constipation. In severe cases, abdominal pain, nausea, and diarrhea can occur.
Viruses
Viruses are made up of a piece of genetic code, such as DNA or RNA, and protected by a coating of protein. Once you’re infected, viruses invade host cells within your body. They then use the components of the host cell to replicate, producing more viruses.
After the replication cycle is complete, these new viruses are released from the host cell. This usually damages or destroys the infected cells.
Some viruses can remain dormant for a time before multiplying again. When this happens, a person appears to have recovered from the viral infection, but gets sick again.
Viruses can cause a number of infections, many of which are contagious. Examples of viral diseases that affects the Liver include:
- Yellow Fever
- Hepatitis A, B, C, D, E
Yellow Fever
Yellow fever is a hemorrhagic condition that can lead to a high fever, bleeding into the skin, and cell death in the liver and kidneys. If enough liver cells die, liver damage occurs, leading to jaundice, a condition in which the skin and eyes takes on a yellowish color. Mosquitoes spread yellow fever. It can affect monkeys and humans. If a mosquito bites a monkey that has the fever, they can pass it to humans. This can lead to outbreaks.
Prevention
In the past, yellow fever devastated communities so scientists developed a safe and effective vaccine that prevents yellow fever.
Vaccination
Anyone traveling to an area where yellow fever is known to exist should find out about having the vaccine at least 10 to 14 days before departure.Some countries may insist on a valid immunization certificate before a person can enter.A single vaccine dose provides at least 10 years’ protection, and the person may be protected for life.
VIRAL HEPATITIS
What is Viral Hepatitis?
Viral hepatitis occurs when a virus causes liver disease or inflamation. the most common hepatitis viruses are hepatitis A virus, hepatitis B virus, hepatitis C virus , hepatitis D virus and hepatitis E.
What is the difference between hepatitis A, hepatitis B, and hepatitis C?
Hepatitis A, hepatitis B, and hepatitis C are liver infections caused by three different viruses. Although each can cause similar symptoms, they are spread in different ways and can affect the liver differently. Hepatitis A is usually a short-term infection and does not become chronic. Hepatitis B and hepatitis C can also begin as short-term, acute infections, but in some people, the virus remains in the body, resulting in chronic disease and long-term liver problems. There are vaccines to prevent hepatitis A and hepatitis B; however, there is no vaccine for hepatitis C.
What is hepatitis A?
Hepatitis A is a highly contagious, short-
term liver infection caused by the hepatitis A virus.
How serious is hepatitis A?
People who get hepatitis A may feel sick for a few weeks to several months but usually recover completely and do not have lasting liver damage. In rare cases, hepatitis A can cause liver failure and even death; this is more common in older people and in people with other serious health issues, such as chronic liver disease.
How is hepatitis A spread?
The hepatitis A virus is found in the stool and blood of people who are infected. The hepatitis A virus is spread when someone
ingests the virus (even in amounts too small to see) through:
►Person-to-person contact
Hepatitis A can be spread from close, personal contact with an infected person, such as through certain types of sexual contact (like oral-anal sex), caring for someone who is ill, or using drugs with others. Hepatitis A is very contagious, and people can even spread the virus before they feel sick.
►Eating contaminated food or drink
Contamination of food with the hepatitis A virus can happen at any point: growing, harvesting, processing, handling, and even after cooking. Contamination of food and
water happens more often in countries where hepatitis A is common. Although uncommon, foodborne outbreaks have occurred from people eating contaminated fresh and frozen imported food products.
What are the symptoms of hepatitis A?
Not everyone with hepatitis A has symptoms. Adults are more likely to have symptoms than children. If symptoms develop, they usually appear 2 to 7 weeks after infection. Symptoms usually last less than 2 months, although some people can be ill for as long as 6 months.
If symptoms develop, they can include:
Yellow skin or eyes
- Not wanting to eat
- Upset stomach
- Throwing up
- Stomach pain
- Fever
- Dark urine or light- colored stools
- Diarrhea
- Joint pain
- Feeling tired
Can a person spread hepatitis A virus without having symptoms?
Yes. Many people, especially children, have no symptoms but can still spread the infection. In addition, a person can transmit the hepatitis A virus to others up to 2 weeks before symptoms appear.
How is hepatitis A treated?
To treat the symptoms of hepatitis A, doctors usually recommend rest, adequate nutrition, and fluids. Some people with severe symptoms will need medical care in a hospital.
How can I protect myself against hepatitis A?
The best way to prevent hepatitis A is through vaccination with the hepatitis A vaccine. To get the full benefit of the hepatitis A vaccine, more than one shot is needed. The number and timing of these shots depends on the type of vaccine you are given. Practicing good hand hygiene — including thoroughly washing hands after using the bathroom, changing diapers, and before preparing or eating food — plays an important role in preventing the spread of hepatitis A.
What is hepatitis B?
Hepatitis B is a liver infection caused by the hepatitis B virus. Some people with hepatitis B are sick for only a few weeks (known as “acute” infection), but for others, the disease progresses to a serious, lifelong illness known as chronic hepatitis B.
What is acute (short-term) hepatitis B?
Acute hepatitis B is a short-term illness that occurs within the first 6 months after someone is exposed to the hepatitis B virus. Some people with acute hepatitis B have no symptoms at all or only mild illness. For others, acute hepatitis B causes a more severe illness that requires hospitalization.
What is chronic (long-term) hepatitis B?
Some people, especially those who get infected in adulthood, are able to clear the virus from their bodies without treatment.
For other people, acute hepatitis B leads to life-long infection known as chronic hepatitis B. Over time, chronic hepatitis B can cause serious health problems, including liver damage, cirrhosis, liver cancer, and even death.
How common is hepatitis B around the world?
An estimated 257 million people are living with hepatitis B worldwide.
How is hepatitis B spread?
Hepatitis B is spread when blood, semen, or other body fluid infected with the hepatitis B virus enters the body of someone who is not infected. People can become infected with the virus from:
Birth (spread from an infected mother to her baby during birth)
- Sex with an infected partner
- Sharing needles, syringes, or drug preparation equipment
- Sharing items such as toothbrushes, razors, or medical equipment (like a glucose monitor) with an infected person
- Direct contact with the blood or open sores of an infected person
- Exposure to an infected person’s blood through needlesticks or other sharp instruments or Blood transfusion
Can a person spread the hepatitis B virus and not know it?
Yes. Many people with hepatitis B don’t know they are infected with the virus because they don’t feel or look sick. However, they can still spread the virus to others.
How long does the hepatitis B virus survive outside the body?
The hepatitis B virus can survive outside the body for at least 7 days. During that time, the virus is still capable of causing infection.
How should blood spills be cleaned from surfaces to make sure that hepatitis B virus is gone?
All blood spills (including those that have already dried) should be cleaned and disinfected with a mixture of bleach and water (1 part household bleach to 10 parts water). Gloves should always be worn when cleaning up any blood spills. Even dried blood can cause infection.
If I have been infected with the hepatitis B virus in the past, can I get it again?
No. If you have been infected with hepatitis B in the past, you can’t get infected again. However, some people, especially those infected during early childhood, remain infected for life because they never cleared the virus from their bodies. These people are considered to have chronic infection and are at risk for developing severe liver disease.
Can I donate blood if I have hepatitis B?
NO! anyone who has tested positive for hepatitis B or anyone experiencing symptoms of viral hepatitis cannot donate.
Can hepatitis B be prevented?
Yes. The best way to prevent hepatitis B is by getting vaccinated. The hepatitis B vaccine is safe and effective. Completing the series of shots (2, 3, or 4 doses, depending on the manufacturer) is needed to be fully protected.
Is it harmful to have an extra dose of hepatitis B vaccine or to repeat the entire hepatitis B vaccine series?
No, getting extra doses of hepatitis B vaccine is not harmful.
What should be done if hepatitis B vaccine series was not completed?
If the hepatitis B vaccine series is interrupted, the next dose should be given as soon as possible. The first dose(s) does not need to be repeated.
Is the hepatitis B vaccine safe?
Yes. The hepatitis B vaccine is safe, and soreness at the injection site is the most common side effect. As with any medicine, there are very small risks that a serious problem could occur after getting the vaccine. The safety of vaccines is always being monitored.
Can I get hepatitis B from being vaccinated?
No. The hepatitis B vaccine does not contain any live virus and can’t cause hepatitis B.
Can I get the hepatitis B vaccine at the same time as other vaccines?
Yes. Getting two different vaccines at the same time is not harmful.
Hepatitis B Symptoms
Does acute (short-term) hepatitis B cause symptoms?
Sometimes. Most children younger than 5 and people with serious health problems (like having compromised immune systems) have no symptoms. Up to half of all older children, adolescents, and adults experience symptoms of acute hepatitis B.
What are the symptoms of acute (short-term) hepatitis B?
Symptoms of acute hepatitis B can include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice (yellow color in the skin or the eyes)
How soon after exposure to the
hepatitis B virus will symptoms appear, and how long do they last?
If symptoms occur, they begin an average of 90 days (or 3 months) after exposure to the virus, but they can appear any time between 8 weeks and 5 months after exposure. They usually last several weeks, but some people can feel sick for as long as 6 months.
Can a person spread hepatitis B without having symptoms?
Yes. Many people with hepatitis B have no symptoms, but they can still spread the virus to others.
What are the symptoms of chronic (long-term) hepatitis B?
Most people with chronic hepatitis B do not have any symptoms, do not feel ill, and remain symptom free for decades. When and if symptoms do appear, they are similar to the symptoms of acute infection, but can be a sign of advanced liver disease. About 1 in 4 people who become chronically infected during childhood and about 15% of those who become chronically infected after childhood will eventually die from serious liver conditions, like cirrhosis (scarring of the liver) or liver cancer. Some people still do not have symptoms even after their liver becomes diseased, although certain blood tests for liver function might show some abnormalities.
How serious is chronic (long-term) hepatitis B?
Chronic hepatitis B can develop into a serious disease resulting in long-term health problems, including liver damage, liver failure, liver cancer, and even death.
Hepatitis B Test
Since many people with hepatitis B do not have symptoms, blood tests are used to diagnose the infection. Several different hepatitis B tests are available. Depending on the test, they can determine whether you have chronic or acute hepatitis B;
- are immune to hepatitis B after vaccination; or
- were infected in the past, have cleared the virus from your body, and are protected from future infection.
Certain tests can even
determine how likely it is that someone who is infected with hepatitis B will transmit it to others.
Treatment
How is chronic hepatitis B treated?
Several medications have been approved to treat people who have chronic hepatitis B, and new drugs are in development.
However, not every person with chronic hepatitis B needs medication, and the drugs may cause side effects in some patients. People who start hepatitis B treatment may need to take medication indefinitely because these medications do not lead to a cure.
What can people with chronic hepatitis B do to take care of their liver?
People with chronic hepatitis B
should be under the care of a health-care provider that is knowledgeable about this illness (like an internist or provider that specializes in treating people with infectious, digestive, or liver diseases) and is able to regularly monitor their liver function. People recently diagnosed with hepatitis B should get vaccinated against hepatitis A and tested for hepatitis C;
- avoid drinking alcohol;
- follow a healthy diet and stay physically active, especially patients who are overweight (i.e., those with body mass index [BMI] ≥25kg/m2) or obese (BMI ≥30kg/m2); and
- check with a health professional before taking any prescription pills, nutritional or herbal
supplements, or over-the-counter medications, as these can potentially damage the liver.
Pregnant Women and their Newborns
Are pregnant women tested for hepatitis B?
Yes. When a pregnant woman comes in for prenatal care, she is given a series of routine
blood tests, including one that checks for hepatitis B virus infection.
If a pregnant woman has hepatitis B, is there a way to prevent her baby from getting hepatitis B?
Yes. Almost all cases of hepatitis B can be prevented in babies born to infected mothers, but these newborns must receive the necessary shots at the recommended times. The combination of hepatitis B immune globulin (known as HBIG) and hepatitis B vaccine can be given to infants born to infected mothers within 12 hours of birth to protect them from infection. To best protect your baby, follow the advice from your baby’s doctor.
Why is the hepatitis B vaccine recommended for all babies?
Nearly all newborns who become infected with the hepatitis B virus develop lifelong hepatitis B. This can eventually lead to serious health problems, including liver damage, liver cancer, and even death. Hepatitis B vaccination is recommended for all babies to protect them from this serious but preventable disease.
What is hepatitis C?
Hepatitis C is a liver infection caused by the hepatitis C virus. Hepatitis C can range from a mild illness lasting a few weeks to a serious, long-term illness. Hepatitis C is often described as “acute,” meaning a new infection, or “chronic,” meaning long-term infection.
- Acute hepatitis C occurs within the first 6 months after someone is exposed to the hepatitis C virus. Hepatitis C can be a short-term illness, but for most people, acute infection leads to chronic infection.
- Chronic hepatitis C can be a lifelong infection if left untreated. Chronic hepatitis C can cause serious health problems, including liver damage, cirrhosis (scarring of the liver), liver cancer, and even death.
How serious is chronic
hepatitis C?
Chronic hepatitis C can be a serious disease resulting in long-term health problems, including liver damage, liver failure, cirrhosis, liver cancer, and even death. It is the most common reason for liver transplantation in the United States
Transmission
How is hepatitis C spread?
The hepatitis C virus is usually spread when someone comes into contact with blood from an infected person. This can happen through:
►Sharing drug-injection equipment.
Today, most people become infected with hepatitis C by sharing needles, syringes, or any other equipment used to
prepare and inject drugs.
►Birth.
Approximately 6% of infants born to infected mothers will get hepatitis C.
►Health care exposures.
Although uncommon, people can become infected when health-care professionals do not follow the proper steps needed to prevent the spread of bloodborne infections.
►Sex with an infected person.
While uncommon, hepatitis C can spread during sex, though it has been reported more often among men who have sex with men.
►Unregulated tattoos or body piercings.
Hepatitis C can spread when getting tattoos or body
piercings in unlicensed facilities, informal settings, or with
non-sterile instruments.
►Sharing personal items.
People can get infected from sharing glucose monitors, razors, nail clippers, toothbrushes, and other items that may have come into contact with infected blood, even in amounts too small to see.
►Blood transfusions and organ transplants.
Before widespread screening of the blood supply in 1992, hepatitis C was also spread through blood transfusions and organ transplants. Now, the risk of transmission to recipients of blood or blood products is extremely low.
Can you get hepatitis C more than once?
Yes. You can be infected again even if you have cleared the virus or were successfully treated and cured. This is why people who currently inject and share needles, syringes, or other drug preparation equipment, along with those who receive maintenance hemodialysis, should be tested for hepatitis C on a regular basis.
Can I get hepatitis C from a mosquito or other insect bite?
No. The hepatitis C virus has not been shown to be transmitted by mosquitoes or other insects.
Symptoms
What are the symptoms of acute (new) hepatitis C?
Many people newly infected with the hepatitis C virus don’t have symptoms, don’t look or feel sick, and therefore don’t know they are infected. For people who develop symptoms, they usually happen 2–12 weeks after exposure to the hepatitis C virus and can include yellow skin or eyes, not wanting to eat, upset stomach, throwing up, stomach pain, fever, dark urine, light-colored stool, joint pain, and feeling tired.
What are the symptoms of chronic (long-term) hepatitis C?
Most people with chronic hepatitis C don’t have any symptoms or have only general
symptoms like chronic fatigue and depression. Many people eventually develop chronic liver disease, which can range from mild to severe and include cirrhosis (scarring of the liver) and liver cancer. Chronic liver disease in people with hepatitis C usually happens slowly, without any signs or symptoms, over several decades. Chronic hepatitis C virus infection is often not recognized until people are screened for blood donation or from an abnormal blood test found during a routine doctor’s visit.
Can a person spread hepatitis C without having symptoms?
Yes. If you are infected with the hepatitis C virus, you can spread it to others even if you have no symptoms.
Can a person have normal liver enzyme level and still have hepatitis C?
Yes. For people with hepatitis C, it is common for liver enzyme levels to go up and down, sometimes returning to normal or near normal. Some people with hepatitis C have liver enzyme levels that are normal for over a year even though they have chronic liver disease.
Treatment
What is the treatment for hepatitis C?
Treatment is recommended for all people,
including non-pregnant women, with acute or chronic hepatitis C (including children aged ≥3 years and adolescents). Current treatments usually involve just 8–12 weeks of oral therapy (pills) and cure over 90% with few side effects.
What can people with chronic hepatitis C do to protect the liver?
People with chronic hepatitis C and those with cirrhosis (even if they have been cured of their hepatitis C infection) should be monitored regularly by a doctor, because these people have a continued risk of complications of advanced liver disease, including liver cancer. In addition, people living with hepatitis C should
- be vaccinated against hepatitis A and hepatitis B
- avoid alcohol because it can cause additional damage to the liver
- check with their doctor before taking any prescription pills, herbs, supplements, or over-the-counter medications, as these can potentially damage the liver
- be tested for HIV, because people who have both infections are more likely to get cirrhosis
Prevention
Is there a vaccine that can prevent hepatitis C?
No. Currently, there is no vaccine to prevent hepatitis C.
What is hepatitis D?
Hepatitis D is a liver infection caused by the hepatitis D virus. Only people infected with the hepatitis B virus can get hepatitis D. They can become infected with both viruses at the same time (known as “coinfection”) or get hepatitis D after first being infected with hepatitis B virus (known as “superinfection”). Hepatitis D can cause severe symptoms and serious illness that can lead to life-long liver damage and even death.
What is hepatitis B/hepatitis D coinfection?
People who get infected with both hepatitis B and hepatitis D at the same time are considered to be coinfected.
Coinfection with hepatitis B and hepatitis D can cause serious, short-term health problems and even liver failure, but it usually does not lead to life-long illness.
What is hepatitis D superinfection?
Superinfection happens when people get hepatitis D after having been first infected with the hepatitis B virus. This type of infection is more likely to result in long-term illness, including rapid development of liver fibrosis, liver failure, and even death.
Where is hepatitis D most common?
Hepatitis D is most common in Eastern Europe, Southern Europe, the Mediterranean region, the Middle East, West and Central Africa, East Asia, and the Amazon Basin in South America.
How is hepatitis D spread?
You can only get hepatitis D after coming into contact with the blood or body fluids of someone who is infected with the hepatitis D virus. This can happen through
- having sex with an infected person
- sharing needles, syringes, or any other equipment used to prepare or inject drugs
- birth to an infected mother (although this is rare)
- contact with blood from the open sores of an infected person
- needle sticks or exposures to sharp instruments
- sharing personal items (e.g., razors and toothbrushes) that may have come in contact with an infected persons blood
What are the signs and symptoms of hepatitis D?
People with hepatitis D can have more severe symptoms than those who are infected with hepatitis B alone. The signs and symptoms of hepatitis D usually appear 3–7 weeks after infection with the hepatitis D virus. They include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored stool
- Joint pain
- Jaundice
How can I prevent hepatitis D?
To prevent hepatitis D, you can get vaccinated against hepatitis B. Although no vaccine is available for hepatitis D, getting the hepatitis B vaccine also protects you from hepatitis D.
What is hepatitis E?
Hepatitis E is a liver disease caused by the hepatitis E virus (HEV). Most people with hepatitis E fully recover and have no long-term liver problems as a result of their infection.
How is hepatitis E spread?
In developing countries, people most often get hepatitis E from drinking water contaminated by feces from people who are infected with the virus. In the United States and other developed countries, people have gotten sick with hepatitis E after eating raw or undercooked pork, venison, and wild boar meat.
How common is hepatitis E?
Hepatitis E is common in many parts of the developing world where sanitation is poor.
Does hepatitis E cause symptoms?
Many people with hepatitis E, especially young children, do not have any symptoms. Others may experience one or more of these symptoms:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored stool
- Joint pain
- Jaundice (a yellowing of the skin or eyes)
How soon after exposure to hepatitis E will symptoms appear?
If symptoms occur, they usually appear anywhere from 2 to 6 weeks after exposure to the virus that causes hepatitis E.
How serious is hepatitis E?
Pregnant women are at greater risk for liver failure and death from hepatitis E. People who have had solid-organ transplants and those with compromised immune systems can experience more severe, long-term liver problems if infected.
How is hepatitis E treated?
There is no specific treatment for hepatitis E. Most people get better by treating their symptoms.
Can hepatitis E be prevented?
No vaccine is available to protect against hepatitis E. However, you can lower your risk for HEV infection by drinking only purified water when visiting countries where hepatitis E is common and by avoiding raw or undercooked pork, venison, and wild boar meat.
WHAT IS FATTY LIVER DISEASE?
Fatty liver is also known as hepatic steatosis. It happens when fat builds up in the liver. Having small amounts of fat in your liver is normal, but too much can become a health problem.Your liver is the second-largest organ in your body. It helps process nutrients from food and drinks, and filters harmful substances from your blood.
Too much fat in your liver can cause liver inflammation, which can damage your liver and create scarring. In severe cases, this scarring can lead to liver failure. When fatty liver develops in someone who drinks a lot of alcohol, it’s known as alcoholic fatty liver disease (AFLD).In someone who doesn’t drink a lot of alcohol, it’s known as nonalcoholic fatty liver disease (NAFLD). Some people with fatty liver disease develop complications, including liver scarring. Liver scarring is known as liver fibrosis. If you develop severe liver fibrosis, it’s known as cirrhosis, a potentially life threatening condition that can cause liver failure.The liver damage due to cirrhosis is permanent. That’s why it’s so important to prevent it from developing in the first place. In people who don’t drink a lot of alcohol, the cause of fatty liver disease may be because their body produces too much fat or doesn’t metabolize fat efficiently enough.
Risk factors
A wide range of diseases and conditions can increase your risk of NAFLD, including:
- High cholesterol
- High levels of triglycerides in the blood
- Metabolic syndrome
- Obesity, particularly when fat is concentrated in the abdomen
- Polycystic ovary syndrome
- Sleep apnea
- Type 2 diabetes
- Underactive thyroid (hypothyroidism)
- Underactive pituitary gland (hypopituitarism)
Prevention
To reduce your risk of NAFLD:
- Choose a healthy diet.Choose a healthy plant-based diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Maintain a healthy weight.If you are overweight or obese, reduce the number of calories you eat each day and get more exercise. If you have a healthy weight, work to maintain it by choosing a healthy diet and exercising.
- Exercise most days of the week. Get an OK from your doctor first if you haven’t been exercising regularly.
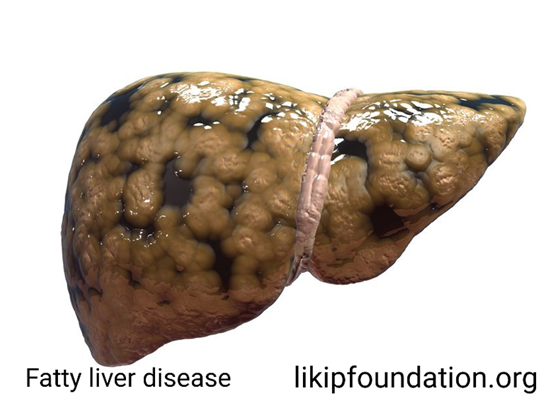
LIVER FIBROSIS
What is Liver Fibrosis?
How Fibrosis Develops
When someone has liver disease, their liver enters into a very dangerous cycle. Persistent inflammation, or hepatitis, sends nonstop signals to repair cells to continue depositing collagen. The extra collagen stiffens around the tissue like it is supposed to in the healthy liver; but, instead of a signal being released to stop the inflammation and discard the extra collagen, the inflammation continues, and even more collagen is deposited, leading to more stiffening. This is how fibrosis develops.When repetitive damage or long-lasting inflammation
occurs, collagen and other proteins build-up between liver cells, forming scar tissue. Scar tissue can block or limit blood flow within the liver, starving and killing healthy liver cells, causing more scar tissue to form. Unlike healthy liver cells, scar tissue cannot function or repair itself. As fibrosis advances it can impact the liver’s ability to function, limit its ability repair itself and restrict blood flow. Over time, the scars in the liver will continue to build and replace healthy tissue. Gradually, the scars snake out farther, covering more of the healthy liver and grow together, or bridge, creating septa or bands of scar tissue. Fibrosis also restricts blood flow. When doctors want to determine how severe the scarring is, they examine the impact on the portal blood flow. The portal vein brings all the blood from the intestines to the liver to be processed.
Fibrosis in mild to moderate stages often does not cause symptoms. Due to a lack of symptoms, many people live with liver damage, or fibrosis, without being diagnosed until they have symptoms of cirrhosis. Fibrosis can be reversed if detected early enough and the underlying liver disease that caused the development of fibrosis can be cured or treated. If fibrosis is left untreated, it can lead to cirrhosis and liver cancer. It is important to remember that the process of fibrosis progressing to cirrhosis happens over a long period of time. The time it takes for fibrosis to progress is different for every disease and every person. Not everyone who develops fibrosis will progress to cirrhosis. Not everyone who gets cirrhosis will get cancer.
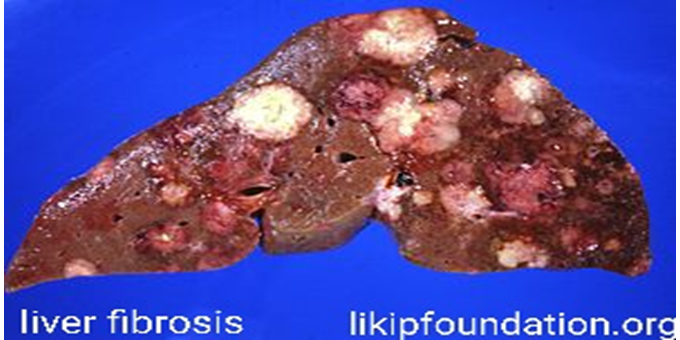
LIVER CIRRHOSIS
What is Liver Cirrhosis?
The final stage of fibrosis is cirrhosis…
Cirrhosis is where your liver is severely scarred and permanently damaged. While the word cirrhosis is most commonly heard when people discuss alcohol-induced liver disease, cirrhosis is caused by many forms of liver disease.
While fibrosis is reversible there is a point where the damage becomes too great and the liver cannot repair itself. There is no
treatment that can cure cirrhosis. If possible, treating the underlying cause of cirrhosis may keep your cirrhosis from getting worse and help prevent liver failure. Successful treatment may slowly improve some of your liver scarring. It is important to avoid things that could damage your liver further like alcohol, certain medications and fatty food. Treatment for someone with cirrhosis often means managing the symptoms of cirrhosis and preventing further damage to avoid liver failure. Doctors treat liver failure with a liver transplant. Someone with cirrhosis is at a very high risk of developing liver cancer. It is very important to receive routine liver cancer surveillance if you have cirrhosis; most people who develop liver cancer have evidence of cirrhosis. Doctors also treat liver cancer with a transplant. It is important to note, people often live with cirrhosis for a long time before the option of liver transplant is discussed.
There is a big difference between liver functioning and disease progression. Our livers are resilient, continuing to function even when they become severely scarred. Because of this, some people may not experience symptoms or have elevated liver enzyme tests even though their liver is damaged. It is important to talk to your doctor about your risks for liver disease so you can receive imaging tests that may help diagnosis liver damage.
Compensated Cirrhosis v. Decompensated Cirrhosis
Cirrhosis is often categorized as either compensated or decompensated.
Someone with compensated cirrhosis doesn’t necessarily look or feel sick. Their symptoms of the disease may be mild or nonexistent even though the liver is severely scarred. Someone with decompensated cirrhosis will feel and appear sick as their liver is struggling to function.
When someone has cirrhosis their liver shrinks and becomes hard, greatly impacting the liver’s ability to process the massive amounts of blood for which it’s responsible. The liver has two sources that supply blood to the liver – the hepatic artery and the hepatic portal vein. The hepatic artery brings oxygen-rich blood into the liver. Blood coming from our digestive system enters the liver through the hepatic portal vein carrying nutrients, medications, or toxins.
When someone has decompensated cirrhosis the scar tissue blocks the blood meant to flow through the portal vein causing an increase of pressure known as portal hypertension. The blood carried in the portal vein is filled with proteins, toxins and other “stuff” meant to be filtered by the liver. The blood unable to enter the liver must find new routes; because the blood is not entering the liver, nutrients, toxins and more from the digestive system does not get properly filtered. Portal hypertension is responsible for symptoms like varices, ascites and encephalopathy. Hepatorenal syndrome can also occur when someone has decompensated cirrhosis.

What is Ascites?
. Ascites (ay-SITE-eez) is when too much fluid builds up in your abdomen (belly). This condition often happens in people who have cirrhosis (scarring) of the liver.
A sheet of tissue called the peritoneum covers the abdominal organs, including the stomach, bowels, liver and kidneys. The peritoneum has two layers. Ascites happens when fluid builds up between the two layers.
What are risk factors for ascites?
Having a condition that causes cirrhosis puts you at greater risk for developing ascites. These conditions include:
- Non-alcohol associated fatty liver disease.
- Hepatitis B.
- Hepatitis C.
- Alcohol use disorder.
- Autoimmune hepatitis.
- Genetic liver diseases like hemochromatosis, Wilson disease and alpha-1-antitrypsin deficiency.
Other conditions that can lead to ascites include:
- Congestive heart failure.
- Kidney failure.
- Cancers of the organs in the abdomen and pelvis.
- Infections.
What causes ascites?
Cirrhosis is the most common cause of ascites. Other conditions that can cause it include heart failure, kidney failure, infection or cancer.
How does cirrhosis cause ascites?
When you have cirrhosis, your liver doesn’t function as it should. The decrease in liver function combines with portal hypertension to cause ascites symptoms. Portal hypertension is high pressure in the portal vein that delivers blood to your liver. The high pressure causes fluid to leak out of your veins into your belly and collect there.
What are the symptoms of ascites?
The main symptoms of ascites are a large belly and rapid weight gain.
Other symptoms include:
- Swelling in your ankles.
- Shortness of breath.
- Digestive issues, such as bloating, abdominal pain, loss of appetite, indigestion and constipation.
- Back pain.
- Difficulty sitting.
- Fatigue.
How is ascites treated?
Limiting sodium in your diet is crucial for treating ascites. For people with ascites, recommended sodium intake is less than 2,000 to 4,000 milligrams a day.
A dietitian can help create a healthy eating plan for you. You may also need to take diuretics (water pills). These water pills help fluid and sodium leave your body.

What is Hepatorenal Syndrome?
The liver is the largest filter in the body but works closely with our kidneys to eliminate waste from our bodies. When someone has cirrhosis, they may develop a serious complication where their kidneys begin to progressively fail. This is called hepatorenal syndrome.
What is Jaundice?
Our red blood cells have a substance in them called hemoglobin which is responsible for carrying oxygen. Bilirubin is a yellow chemical found in hemoglobin. Your body builds new cells to replace broken down red blood cells and the old ones are processed in the liver. The breakdown of the old cells releases bilirubin. A healthy liver processes bilirubin out of the body. If the liver cannot successfully do this function, bilirubin builds up in the body and your skin or the whites or your eyes may look yellow. This is called jaundice.
This buildup of bilirubin can also cause someone’s urine to become very dark or their poop to be pale in color. Excess bilirubin is excreted in urine which causes someone’s pee to look very dark and brown, almost like a cola soda. The lack of bilirubin entering the gut causes someone’s stool to be very light in color. Jaundice does not only occur in people with cirrhosis. Many healthy babies have
jaundice during the first week of life. Jaundice can also be due to blood diseases, genetic conditions, blockages of bile ducts, infections (like hepatitis A), and even some medications.
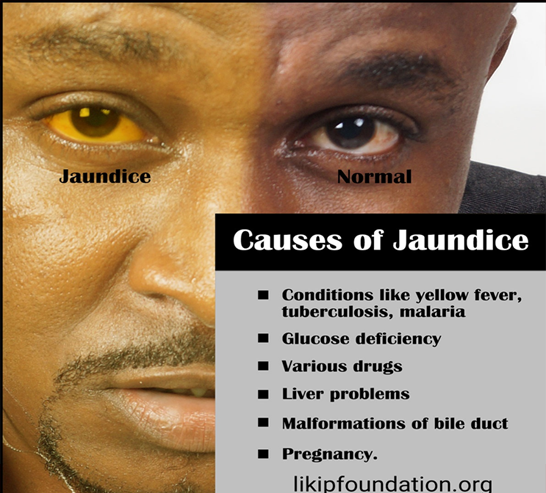
What is Gallstones?
Gallstones are hardened deposits of digestive fluid that can form in your gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder holds a digestive fluid called bile that’s released into your small intestine. Gallstones range in size from as small as a grain of sand to as large as a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time.
Symptoms
Gallstones may cause no signs or symptoms. If a gallstone lodges in a duct and causes a blockage, the resulting signs and symptoms may include:
- Sudden and rapidly intensifying pain in the upper right portion of your abdomen
- Sudden and rapidly intensifying pain in the center of your abdomen, just below your breastbone
- Back pain between your shoulder blades
- Pain in your right shoulder
- Nausea or vomiting
Gallstone pain may last several minutes to a few hours.
Types of gallstones
Types of gallstones that can form in the gallbladder include:
- Cholesterol gallstones.The most common type of gallstone, called a cholesterol gallstone, often appears yellow in color. These gallstones are composed mainly of undissolved cholesterol, but may contain other components.
- Pigment gallstones.These dark brown or black stones form when your bile contains too much bilirubin.
Risk factors
Factors that may increase your risk of gallstones include:
- Being female
- Being age 40 or older
- Being overweight or obese
- Being sedentary
- Being pregnant
- Eating a high-fat diet
- Eating a high-cholesterol diet
- Eating a low-fiber diet
- Having a family history of gallstones
- Having diabetes
- Having certain blood disorders, such as sickle cell anemia or leukemia
- Losing weight very quickly
- Taking medications that contain estrogen, such as oral contraceptives or hormone therapy drugs
- Having liver disease
Complications
Complications of gallstones may include:
- Inflammation of the gallbladder.A gallstone that becomes lodged in the neck of the gallbladder can cause inflammation of the gallbladder (cholecystitis). Cholecystitis can cause severe pain and fever.
- Blockage of the common bile duct.Gallstones can block the tubes (ducts) through which bile flows from your gallbladder or liver to your small intestine. Severe pain, jaundice and bile duct infection can result.
- Blockage of the pancreatic duct.The pancreatic duct is a tube that runs from the pancreas and connects to the common bile duct just before entering the duodenum. Pancreatic juices, which aid in digestion, flow through the pancreatic duct.
A gallstone can cause a blockage in the pancreatic duct, which can lead to inflammation of the pancreas (pancreatitis). Pancreatitis causes intense, constant abdominal pain and usually requires hospitalization.
- Gallbladder cancer.People with a history of gallstones have an increased risk of gallbladder cancer. But gallbladder cancer is very rare, so even though the risk of cancer is elevated, the likelihood of gallbladder cancer is still very small.
Prevention
You can reduce your risk of gallstones if you:
- Don’t skip meals.Try to stick to your usual mealtimes each day. Skipping meals or fasting can increase the risk of gallstones.
- Lose weight slowly.If you need to lose weight, go slow. Rapid weight loss can increase the risk of gallstones. Aim to lose 1 or 2 pounds (about 0.5 to 1 kilogram) a week.
- Eat more high-fiber foods.Include more fiber-rich foods in your diet, such as fruits, vegetables and whole grains.
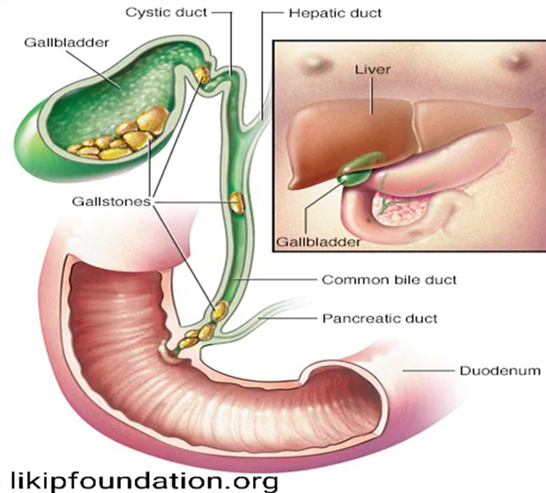
Maintain a healthy weight.
Obesity and being overweight increase the risk of gallstones. Work to achieve a healthy weight by reducing the number of calories you eat and increasing the amount of physical activity you get. Once you achieve a healthy weight, work to maintain that weight by continuing your healthy diet and continuing to exercise.
What is Esophageal Varices?
When blood cannot flow through the portal vein into the liver it is forced to find new pathways, such as through the veins in the stomach and esophagus. These enlarged veins are called varices. These small veins are not meant to carry so much blood. When overloaded with blood, these veins can balloon, leak blood or even rupture, causing life-threatening bleeding. Varices usually don’t cause any symptoms unless they bleed. Signs of bleeding varices include:
- Vomiting large amounts of blood
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness (in severe cases)
Doctors can view these varices by inserting an endoscope (a thin flexible tube) through your mouth, down to your esophagus and stomach. Endoscopies are very important to avoid varices from bursting and bleeding. Doctors use endoscopies to check on the varices and, if needed, band them, or tie them off, to strangle the vein and keep them from bursting.
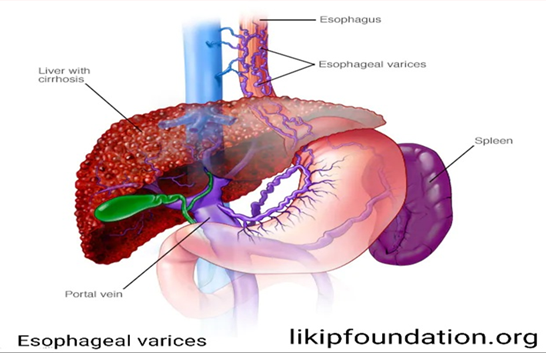
LIVER CANCER
What is Liver Cancer?
Liver cancer is cancer that begins in the cells of your liver. While several types of cancer can form in the liver, the most common type of liver cancer is hepatocellular carcinoma, or HCC, which begins in the main type of liver cells (hepatocytes). Liver cancer is one of the leading causes of cancer-related deaths worldwide. While most other common cancers have seen improved survival rates during this time period, liver cancer death rates have doubled.
It is very rare to develop HCC without first having cirrhosis. Because of this, when someone has been diagnosed with advanced fibrosis (F3) or cirrhosis they should receive regular surveillance for liver cancer. Finding and diagnosing liver cancer as soon as possible is essential. Early detection offers more potentially curative options, like resection (where the cancer and surrounding liver tissue is removed) and transplant.
What Causes Liver Cancer?
Primary liver cancer (hepatocellular carcinoma) tends to occur in livers damaged by birth defects, alcohol abuse, or chronic infection with diseases such as hepatitis B and C, hemochromatosis (a hereditary disease associated with too much iron in the liver), and cirrhosis. More than half of all people diagnosed with primary liver cancer have cirrhosis — a scarring condition of the liver commonly caused by alcohol abuse. Hepatitis B and C and hemochromatosis can cause permanent damage and liver failure. Liver cancer may also be linked to obesity and fatty liver disease.
Various cancer-causing substances are associated with primary liver cancer, including certain herbicides and chemicals such as vinyl chloride and arsenic. Smoking, especially if you abuse alcohol as well, also increases risk. Aflatoxins, cancer-causing substances made by a type of plant mold, have also been implicated. Aflatoxins can contaminate wheat, peanuts, rice, corn, and soybeans. These are rare problems in most developed countries like the U.S. Other causes include the hormones androgen and estrogen and a dye formerly used in medical tests called thorotrast.
Other risk factors for liver cancer may include:
- Your sex. Men are more likely to get hepatocellular carcinoma than women.
- Your weight.Obesity can increase the risk for hepatocellular carcinoma.
- Your race. In the U.S., liver cancer is most common in Asian Americans and Pacific Islanders.
- Anabolic steroid use. Male hormones abused by athletes to increase muscle can slightly increase liver cancer risk with long-term use.
- History of diabetes. Studies have suggested a link between diabetes and liver cancer. This is likely due to the link between diabetes and fatty liver disease.
- Inherited metabolic diseases. Diseases that disrupt the normal metabolism of the body have been shown to increase your risk of liver cancer.
- Rare diseases. Studies have found a link between liver cancer and some rare diseases like alpha -1-antitrypsin deficiency, tyrosinemia, and Wilson’s disease.
What Are the Symptoms of Liver Cancer?
Liver cancer usually has no initial symptoms or may have vague symptoms such as fatigue, fever, chills, and night sweats. Eventually, symptoms may include:
- Pain, swelling, or tenderness in the upper right section of the abdomen
- Weight loss
- Loss of appetite
- Jaundice — yellowing of the skin and whites of the eyes
- Itching all over the body
- Swollen legs
In the advanced stage, symptoms may include fever, nausea, vomiting, fatigue, general weakness, mental confusion, loss of sex drive, pain in the left side of the abdomen due to an enlarged spleen, and the development of skin lesions that resemble a spider.
What Are the Treatments for Liver Cancer?
Any liver cancer is difficult to cure. Primary liver cancer is rarely detectable early, when it is most treatable. Secondary or metastatic liver cancer is hard to treat because it has already spread. The liver’s complex network of blood vessels and bile ducts makes surgery difficult. Most treatment concentrates on making patients feel better and perhaps live longer.Patients with early-stage tumors that can be removed surgically have the best chance of long-term survival. Unfortunately, most liver cancers are inoperable at the time it’s diagnosed, either because the cancer is too advanced or the liver is too diseased to permit surgery
How Can I Prevent Liver Cancer?
Here are ways to reduce your risk of getting liver cancer:
- If you risk exposure to hepatitis, ask your doctor about getting immunized.
- Practice safe sex and avoid IV drug use.
- Drink alcohol only in moderation.
- If you work around chemicals linked to liver cancer, follow safety guidelines to avoid unnecessary contact.
- Before taking iron supplements, check with a doctor to make sure you really need them.
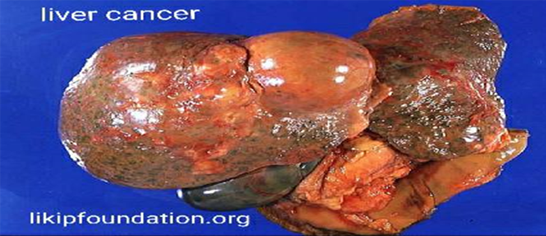
- Do not use anabolic steroids unless medically necessary.
.
Healthy Liver Tips
there are many other things patients can do to protect their liver and improve their health. Below is our list of the top 10 healthy choices that can be started today!
- Schedule regular visits with your liver specialist or health care provider to stay on top of your health and the health of your liver.
- Get the Hepatitis A vaccine to protect yourself from another virus that attacks the liver.
- Avoid drinking alcohol and smoking since both will hurt your liver, which is already being injured by the hepatitis B virus.
- Talk to your Doctor before starting any herbal remedies or vitamin supplements because some could interfere with your prescribed hepatitis B drugs or even damage your liver.
- Check with your pharmacist about any over-the-counter drugs (e.g. acetaminophen, paracetamol) or non-hepatitis B prescription drugs before taking them to make sure they are safe for your liver since many of these drugs are processed through your liver.
- Avoid inhaling fumes from paint, paint thinners, glue, household cleaning products, nail polish removers, and other potentially toxic chemicals that could damage your liver.
- Eat a healthy diet of fruit, whole grains, fish and lean meats, and lot of vegetables. “Cruciferous vegetables” in particular — cabbage, broccoli, cauliflower — have been shown to help protect the liver against environmental chemicals.
- Limit foods and drinks with added sugars including sodas, fruit juices, desserts, packaged snacks and other foods that contain added sugar.
- Limit foods containing saturated fats including fatty cuts of meat and foods fried in oil.
- Avoid eating raw or undercooked shellfish (e.g. clams, mussels, oysters, scallops) because they could be contaminated with a bacteria called Vibrio vulnificus, which is very toxic to the liver and could cause a lot of damage.
- Check for signs of mold on nuts, maize, corn, groundnut, sorghum, and millet before using these foods. Mold is more likely to be a problem if food is stored in damp conditions and not properly sealed. If there is mold, then the food could be contaminated by “aflatoxins,” which are a known risk factor for liver cancer.
- Reduce your stress levels by eating healthy foods, exercising regularly, and getting plenty of rest.
Keep in mind everything you eat, drink, breathe, or absorb through the skin is eventually filtered by the liver. So protect your liver and your health.
Share this page to educate others or click on the whatsapp below to talk to our Doctor