Kidney
About the Kidneys
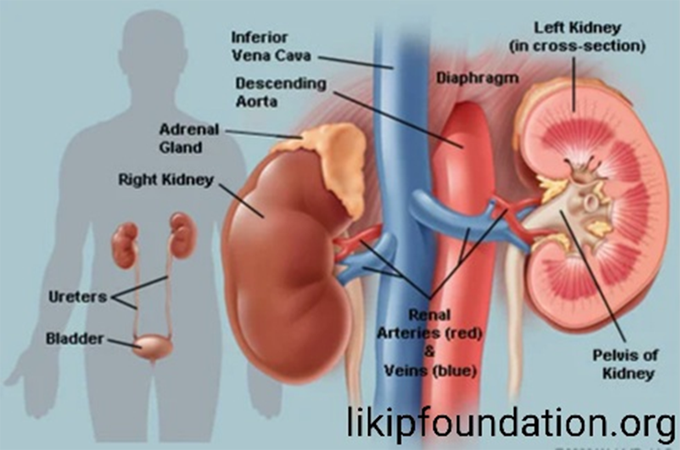
The kidneys are two bean-shaped organs about the size of an adult fist that sit below the ribs towards the middle of the back. They are vital for good health: their main job is to clean the blood by removing excess water and waste, and passing them out of the body in the form of urine. Narrow tubes called ureters carry urine from the kidneys to the bladder.
Each day the kidneys will filter between 150 and 180 litres of blood and pass around two litres of waste down to the bladder. They make sure blood pressure is stable and that there is a stable balance of salts and other substances in the blood. They also produce hormones that help build strong bones and form red blood cells.
When a kidney is not working properly waste products such as salts can build up inside the body and cause health problems. These can become serious or even life-threatening.
We are thought to have two kidneys because they are so crucial to our survival, the second is considered to perhaps be a ‘back up’.
What Your Kidneys Do
Healthy kidneys:
- Keep a balance of water and minerals (such as sodium, potassium, and phosphorus) in your blood
- Remove waste from your blood after digestion, muscle activity, and exposure to chemicals or medications
- Make renin, which your body uses to help manage your blood pressure
- Make a chemical called erythropoietin, which prompts your body to make red blood cells
- Make an active form of vitamin D, needed for bone health and other things
Kidney Disease And Causes
If your kidneys suddenly stop working, doctors call it acute kidney injury or acute renal failure. The main causes are:
- Not enough blood flow to the kidneys
- Direct damage to the kidneys
- Urine backed up in the kidneys
Those things can happen when you:
- Have a traumatic injury with blood loss, such as in a car wreck
- Are dehydrated or your muscle tissue breaks down, sending too much protein into your bloodstream
- Go into shock because you have a severe infection called sepsis
- Have an enlarged prostate that blocks your urine flow
- Take certain drugs or are around certain toxins that directly damage the kidney
- Have complications during a pregnancy, such as eclampsia and preeclampsia
- Autoimmune diseases — when your immune system attacks your body — can also cause an acute kidney injury.
- People with severe heart or liver failure commonly go into acute kidney injury as well.
Chronic kidney disease causes:
When your kidneys don’t work well for longer than 3 months, doctors call it chronic kidney disease. You may not have any symptoms in the early stages, but that’s when it’s simpler to treat. Diabetes (types 1 and 2) and high blood pressure are the most common culprits. High blood sugar levels over time can harm your kidneys. And high blood pressure creates wear and tear on your blood vessels, including those that go to your kidneys. Other causes include: Medication Errors, immune system disease, Viral infections or bacterial infections ( Pyelonephritis), high cholesterol, Glomerulonephritis, polycystic kidney disease, birth defects, Drugs and toxins , kidney stones etc.
# Prescription/medication Errors.
A medication error is defined as “any preventable event that may cause or lead
to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer,”
Medication errors can occur throughout the medication-use system. Such as, when prescribing a drug, upon entering information into a computer system, when the drug is being prepared or dispensed, or when the drug is given to or taken by a patient. So Doctors, nurses, pharmacists or Medicine Counter Assistants, care givers and patients are all involved.
Medication errors refer to mistakes in prescribing, dispensing and giving medications. They injure hundreds of thousands of people every year in the United States. Yet most medication errors can be prevented. How can you protect yourself and your family?
One of the best ways to reduce your risk of a medication error is to take an active role in your own health care. Learn about the medications you take — including possible side effects. Never hesitate to ask questions or share concerns with your doctor, pharmacist and other health care providers.
What exactly are medication errors?
Medication errors are preventable events due to the inappropriate use of medications. Medication errors that cause harm are called preventable adverse drug events. If a medication error occurred, but didn’t hurt anyone, it’s called a potential adverse drug event. An example of a medication error is taking an over-the-counter product that contains acetaminophen (Tylenol, others) when you’re already taking a prescription pain medicine that contains this exact ingredient. This mistake could cause you to take more than the recommended dose of acetaminophen, putting yourself at risk of liver damage.
Another example of a possible medication error is taking a depression medication called fluoxetine (Prozac, Sarafem) with a migraine drug called sumatriptan (Imitrex). Both medicines affect levels of a brain chemical called serotonin. Taking them together may lead to a potentially life-threatening condition called serotonin syndrome. Symptoms of the dangerous drug interaction include confusion, agitation, rapid heartbeat and increased
body temperature, among others.
How do medication errors happen?
Medication errors can happen to anyone in any place, including your own home and at the doctor’s office, hospital, pharmacy and senior living facility. Kids are especially at high risk for medication errors because they typically need different drug doses than adults.
Knowing what you’re up against can help you play it safe. The most common causes of medication errors are:
- Poor communication between your doctors
- Poor communication between you and your doctors
- Drug names that sound alike and medications that look alike
- Medical abbreviations
- Patient names that look alike
- Unclear hand writing from Doctors
Know how to prevent medication errors
Knowledge is your best defense. If you don’t understand something your doctor says, ask for an explanation. Whenever you start a new medication, make sure you know the answers to these questions:
- What is the brand or generic name of the medication?
- What is the medication supposed to do? How long will it be until I see results?
- What is the dose? How long should I take it?
- What should I do if I miss a dose?
- What should I do if I accidentally take more than the recommended dose?
- Are there any foods, drinks, other medications or activities I should avoid while taking this medicine?
- What are the possible side effects? What should I do if they occur?
- Will this new medication interfere with my other medication(s)? If so, how?
Your doctor can help prevent medication errors by using a computer to enter and print (or digitally send) any prescription details, instead of hand writing one.
Participate in medication reconciliation
Asking questions is essential, but it isn’t enough. Your Doctor can follow a process called medication reconciliation to significantly decrease your risk of medication errors.
Medication reconciliation is a safety strategy that involves comparing the list of medications your Doctor currently has with the list of medications you are currently taking. This process is done to avoid medication errors such as:
- Missing medications (omissions)
- Duplicate medications
- Dosing errors
- Drug interactions
Medication reconciliation should be done at every transition of care in which new medications are ordered or existing orders are rewritten. Transitions in care include changes in setting (such as being admitted or discharged from the hospital), health care provider or level of care.
Sharing your most up-to-date information with your health care providers gives the
clearest picture of your condition and helps avoid medication mistakes.
Here’s what you need to tell your health care providers:
- The name and strength of all medications you’re taking and when you take them, including prescription medications, herbs, vitamins, nutritional supplements, over-the-counter drugs, vaccines and anything received intravenously, including diagnostic and contrast agents, radioactive medications, feeding tube supplements and blood products
Any medications that you’re allergic to or that have caused problems for you in the past
- Whether you have any chronic or serious health problems
- If you might be pregnant or you’re trying to become pregnant
Avoid these mistakes
The following medication errors have happened to some people. Don’t make these same mistakes:
- Confusing eardrops and eyedrops.Always double-check the label. If a medication says “otic,” it’s for the ears. If it says “ophthalmic,” it’s for the eyes.
- Chewing nonchewables.Don’t assume chewing a pill is as good as swallowing it. Some medications should never be chewed, cut or crushed. Doing so may change how they’re absorbed by the body.
- Cutting up pills.Never split pills unless your doctor or pharmacist has told you it’s safe to do so. Some medications shouldn’t be cut because they’re specially coated to be long acting or to protect the stomach.
- Using the wrong spoon.The spoons in your silverware drawer aren’t measuring spoons. To get an accurate dose, use an oral syringe (available at pharmacies) or the dose cup that came with the medication.
Make safety a habit
Get into the habit of playing it safe with these medication tips:
- Keep an up-to-date list of all your medications, including nonprescription drugs and supplements.
- Store medications in their original labeled containers.
- Keep your medications organized by using a pillbox or an automatic pill dispenser.
- Save the information sheets that come with your medications.
Use the same pharmacy, if possible, for all of your prescriptions.
- When you pick up a prescription, check that it’s the one your doctor ordered.
- Don’t give your prescription medication to someone else and don’t take someone else’s.
A final word on medication errors
“Don’t ask, don’t tell” is never a smart policy when it comes to medications and your health. Don’t hesitate to ask questions or to tell your health care providers if anything seems amiss. Remember, you’re the final line of defense against medication errors.
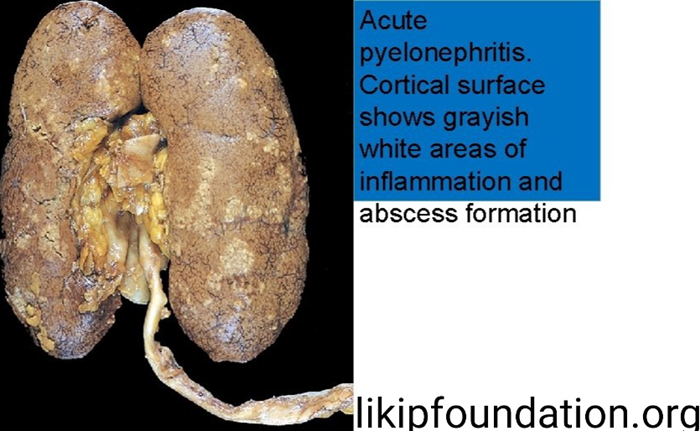
# PYELONEPHRITIS
What Is a Pyelonephritis or Kidney Infection?
A kidney infection, also called pyelonephritis, is when bacteria or viruses cause problems in one or both of your kidneys. It’s a type of urinary tract infection (UTI).
Your kidneys’ main job is to remove waste and take extra water from your blood. They’re part of your urinary tract, which makes liquid waste (urine) and removes it from your body. Like the exhaust system on your car, you want everything to work like it should so waste moves in one direction only: out.
Your urinary tract is made up of your:
- Kidneys. These clean waste from your blood and make urine (your pee).
- Ureters. These thin tubes, one for each kidney, carry urine to your bladder.
- Bladder. This stores urine.
- Urethra. This tube carries urine from your bladder to outside your body.
If any of these parts gets germs in it, you can get a UTI. Most often, your bladder gets infected first. This can be painful .But if the bad bacteria or viruses travel up your ureters, you can get a kidney infection. If left untreated, a kidney infection can cause life-threatening problems. Although the urinary system is designed to keep bacteria out, problems can occur. Escherichia coli (E.coli) or other bacteria found in the intestines can enter the urinary tract through the urethra. These bacteria can travel up into the bladder. When this happens it can cause cystitis (inflammation of the bladder). It can also cause a urinary tract infection (UTI). Cystitis occurs in 1-3% of adult women per year. If the infection continues up to the kidneys, it can cause kidney infection. About 1 in every 30 cases of UTI leads to a kidney infection.
Kidney Infection Symptoms
Symptoms of a kidney infection include:
- Blood or pus in your pee
- Fever and chills
- Loss of appetite
- Pain in your lower back, side, or groin
- Upset stomach or vomiting
- Weakness or fatigue
You may also have some of the symptoms of a bladder infection, such as:
- Burning or pain when you pee
- A constant urge to pee, even soon after you empty your bladder
- Cloudy or bad-smelling urine
- Pain in your lower belly
- Peeing much more often than usual
Call your doctor if you have these symptoms, especially if you have a bladder infection and you’re not getting better.
Kidney Infection Causes
Kidney infections usually start with a bladder infection that spreads to your kidney. Bacteria called E. coli are most often the cause. Other bacteria or viruses can also cause kidney infections.
It’s rare, but an infection can also get in through your skin, make its way into your blood, and travel to your kidney. You can get an infection after kidney surgery, too, but that’s even more unlikely.
Kidney Infection Risk Factors
Anyone can get a kidney infection. But just as women get more bladder infections than men, they also get more kidney infections.
A woman’s urethra is shorter than a man’s, and it’s closer to their vagina and anus. That means it’s easier for bacteria or viruses to get into a woman’s urethra, and once they do, it’s a shorter trip to the bladder. From there, they can spread to the kidneys.
Pregnant women are even more likely to get bladder infections. This is because of hormone changes and because a baby puts pressure on the mother’s bladder and ureters and slows the flow of urine.
Any problem in your urinary tract that keeps pee from flowing as it should can raise your chances of a kidney infection, such as:
- A blockage in your urinary tract, like a kidney stone or enlarged prostate
- Conditions that keep your bladder from completely emptying
- A problem in the structure of your urinary tract, like a pinched urethra
- Vesicoureteral reflux (VUR), which is when pee flows backward from your bladder toward your kidneys
You’re also more likely to get an infection if you have:
- Nerve damage in your bladder
- A prostate infection, known as prostatitis
- A urinary catheter, a tube that goes into your bladder through your urethra to drain pee
- A weakened immune system, as with type 2 diabetes
Kidney Infection Diagnosis
After asking about your symptoms, your doctor will probably do tests including:
- Urine analysis to check for blood, pus, and bacteria in your pee
- Urine culture to see what kind of bacteria you have
Your doctor may also use these tests:
- Ultrasound or CT. These look for a blockage in your urinary tract. Your doctor might do these if treatment doesn’t help within 3 days.
- Voiding cystourethrogram (VCUG). This is a type of X-ray to look for problems in your urethra and bladder. Doctors often use these in children who have VUR.
- Digital rectal exam (for men). Your doctor inserts a lubricated finger into your anus to check for a swollen prostate.
- Dimercaptosuccinic acid (DMSA) scintigraphy. This uses a radioactive material to show kidney infection and damage.
Kidney Infection Complications
If you don’t get treatment, a kidney infection can cause serious problems like:
- Kidney damage. Pus might collect and create an abscess inside the kidney tissue. The bacteria may spread to other parts of your body. Your kidneys can also become scarred, which can lead to high blood pressure, chronic kidney disease, and kidney failure.
- Blood poisoning (septicemia). When bacteria from a kidney infection get into your blood, they can spread through your body and into your organs. This is a medical emergency and needs treatment right away.
- Severe infection. An infection called emphysematous pyelonephritis (EPN) may destroy kidney tissue and make toxic gas build up there. It usually happens in people who have diabetes.
- Problems in pregnancy. Women who have kidney infections while pregnant are more likely to have babies born early or at a low weight. They’re also more likely to have kidney complications.
Kidney Infection Treatment
Your doctor will probably prescribe antibiotics, which you may need for a week or two. Your symptoms should improve within a few days, but make sure to take all of the medicine.
If you have a severe infection, you’ll need to stay in the hospital and get antibiotics intravenously (IV), through a needle.
If your kidney infections keep coming back, there might be a problem with the structure of your urinary tract. Your doctor may send you to a specialist, such as a urologist. These types of issues often need surgery.
Kidney Infection Home Remedies
You can do some things at home to feel better while you have an infection:
- Drink plenty of fluids to flush out germs.
- Get extra rest.
- When you go to the bathroom, sit on the toilet instead of squatting over it, which can keep your bladder from completely emptying.
Don’t use aspirin, ibuprofen, or naproxen because these can raise your risk of kidney problems.
- Use a heating pad on your belly, back, or side.
Kidney Infection Prevention
You can’t completely prevent bladder infections. But you may be less likely to get one if you:
- Don’t use deodorant sprays or douches on your genitals.
- Don’t use condoms or diaphragms with spermicide, which can trigger bacteria growth.
- Use lubricated condoms. Other kinds can irritate the urethra, which makes infection more likely.
- Drink lots of water.
- Go to the bathroom as soon as you feel the urge.
- Pee after having sex.
- Wipe front to back after using the bathroom.
# Glomerulonephritis
What is Glomerulonephritis?
Glomerulonephritis affects tiny structures found in the kidneys called glomeruli. Glomeruli filter the blood. When they become diseased, the body has difficulty getting rid of waste products and excess water. In severe cases, it leads to kidney failure.
Glomerulonephritis is inflammation of the tiny filters in your kidneys (glomeruli). Glomeruli remove excess fluid, electrolytes and waste from your bloodstream and pass them into your urine. Glomerulonephritis can come on suddenly (acute) or gradually (chronic).
Causes
Many conditions can cause glomerulonephritis. Sometimes the disease runs in families and sometimes the cause is unknown. Conditions that can lead to inflammation of the kidneys’ glomeruli include:
Infections
- Post-streptococcal glomerulonephritis.Glomerulonephritis may develop a week or two after recovery from a strep throat infection or, rarely, a skin infection (impetigo). To fight the infection, your body produces extra antibodies that can eventually settle in the glomeruli, causing inflammation.
Children are more likely to develop post-streptococcal glomerulonephritis than are adults, and they’re also more likely to recover quickly.
- Bacterial endocarditis.Bacteria occasionally can spread through your bloodstream and lodge in your heart, causing an infection of one or more of your heart valves. You’re at greater risk of this condition if you have a heart defect, such as a damaged or artificial heart valve. Bacterial endocarditis is associated with glomerular disease, but the connection between the two is unclear.
- Viral infections.Viral infections, such as the human immunodeficiency virus (HIV), hepatitis B and hepatitis C, can trigger glomerulonephritis.
Immune diseases (Lupus). A chronic inflammatory disease, lupus can affect many parts of your body, including your skin, joints, kidneys, blood cells, heart and lungs.
- Goodpasture’s syndrome.A rare immunological lung disorder that can mimic pneumonia, Goodpasture’s syndrome causes bleeding in your lungs as well as glomerulonephritis.
- IgA nephropathy.Characterized by recurrent episodes of blood in the urine, this primary glomerular disease results from deposits of
immunoglobulin A (IgA) in the glomeruli. IgA nephropathy can progress for years with no noticeable symptoms.
Vasculitis Polyarteritis. This form of vasculitis affects small and medium blood vessels in many parts of your body, such as your heart, kidneys and intestines.
- Granulomatosis with polyangiitis.This form of vasculitis, formerly known as Wegener’s granulomatosis, affects small and medium blood vessels in your lungs, upper airways and kidneys.
Symptoms
Signs and symptoms of glomerulonephritis depend on whether you have the acute or chronic form and the cause. Your first indication that something is wrong might come from symptoms or from the results of a routine urinalysis.
Glomerulonephritis signs and symptoms include:
- Pink or cola-colored urine from red blood cells in your urine (hematuria)
- Foamy urine due to excess protein (proteinuria)
- High blood pressure (hypertension)
- Fluid retention (edema) with swelling evident in your face, hands, feet and abdomen
Complications
Glomerulonephritis can damage your kidneys so that they lose their filtering ability. As a result, dangerous levels of fluid, electrolytes and waste build up in your body.
Possible complications of glomerulonephritis include:
- Acute kidney failure.Loss of function in
the filtering part of the nephron can result in rapid accumulation of waste products. You might need emergency dialysis — an artificial means of removing extra fluids and waste from your blood — typically by an artificial kidney machine.
- Chronic kidney disease.Your kidneys gradually lose their filtering ability. Kidney function that deteriorates to less than 10 percent of normal capacity results in end-stage kidney disease, which requires dialysis or a kidney transplant to sustain life.
- High blood pressure.Damage to your kidneys and the resulting buildup of wastes in the bloodstream can raise your blood pressure.
- Nephrotic syndrome.With this syndrome, too much protein in your urine results in too little protein in your blood. Nephrotic syndrome can be associated with high blood cholesterol and swelling (edema) of the eyelids, feet and abdomen.
Prevention
There may be no way to prevent most forms of glomerulonephritis. However, here are some steps that might be beneficial:
- Seek prompt treatment of a strep infection with a sore throat or impetigo.
- To prevent infections that can lead to some forms of glomerulonephritis, such as HIV and hepatitis, follow safe-sex guidelines and avoid intravenous drug use.
- Control high blood pressure, which lessens the likelihood of damage to your kidneys from hypertension.
- Control your blood sugar to help prevent diabetic nephropathy.
# Birth Defects can block the urinary tract or affect the kidneys. One of the most common ones involves a kind of valve between the bladder and urethra.
# Drugs and toxins — such as lead poisoning, long-term use of some medications including NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen and naproxen, and IV street drugs — can permanently damage your kidneys. So can being around some types of chemicals over time.
# Kidney stones
What is kidney Stone?
Kidney stones are materials in the urine that stick together and become hard. Sometimes urine contains so much waste material that it crystallises to form small
stones in the kidney. Most people’s urine contains chemicals that stop the crystals from forming. However, in some cases, these chemicals do not work efficiently.
Kidney stones (also called renal calculi, nephrolithiasis or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys.
Diet, excess body weight, some medical conditions, and certain supplements and medications are among the many causes of kidney stones. Kidney stones can affect any part of your urinary tract — from your kidneys to your bladder. Often, stones form when the urine becomes concentrated, allowing minerals to crystallize and stick together.
Passing kidney stones can be quite painful, but the stones usually cause no
permanent damage if they’re recognized in a timely fashion. Depending on your situation, you may need nothing more than to take pain medication and drink lots of water to pass a kidney stone. In other instances — for example, if stones become lodged in the urinary tract, are associated with a urinary infection or cause complications — surgery may be needed.
Your doctor may recommend preventive treatment to reduce your risk of recurrent kidney stones if you’re at increased risk of developing them again.
What are kidney stone Symptoms?
A kidney stone usually will not cause symptoms until it moves around within your kidney or passes into your ureters — the tubes connecting the kidneys and the bladder. If it becomes lodged in the ureters, it may block the flow of urine and cause the kidney to swell and the ureter to spasm, which can be very painful. At that point, you may experience these signs and symptoms:
- Severe, sharp pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain or burning sensation while urinating
Other signs and symptoms may include:
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- A persistent need to urinate, urinating more often than usual or urinating in small amounts
- Nausea and vomiting
- Fever and chills if an infection is present
Pain caused by a kidney stone may change — for instance, shifting to a different location or increasing in intensity — as the stone moves through your urinary tract.
What Causes kidney stones?
Kidney stones often have no definite, single cause, although several factors may increase your risk.
Kidney stones form when your urine contains more crystal-forming substances — such as calcium, oxalate and uric acid — than the fluid in your urine can dilute. At the same time, your urine may lack substances that prevent crystals from sticking together, creating an ideal environment for kidney stones to form.
Types of kidney stones
Knowing the type of kidney stone you have helps determine its cause, and may give
clues on how to reduce your risk of getting more kidney stones. If possible, try to save your kidney stone if you pass one so that you can bring it to your doctor for analysis.
Types of kidney stones include:
- Calcium stones.Most kidney stones are calcium stones, usually in the form of calcium oxalate. Oxalate is a substance made daily by your liver or absorbed from your diet. Certain fruits and vegetables, as well as nuts and chocolate, have high oxalate content.
Dietary factors, high doses of vitamin D, intestinal bypass surgery and several metabolic disorders can increase the concentration of calcium or oxalate in urine.
Calcium stones may also occur in the form of calcium phosphate. This type of stone is more common in metabolic conditions, such as renal tubular acidosis. It may also be associated with certain medications used to treat migraines or seizures, such as topiramate (Topamax, Trokendi XR, Qudexy XR).
- Struvite stones.Struvite stones form in response to a urinary tract infection. These stones can grow quickly and become quite large, sometimes with few symptoms or little warning.
- Uric acid stones.Uric acid stones can form in people who lose too much fluid because of chronic diarrhea or malabsorption, those who eat a high-protein diet, and those with diabetes or metabolic syndrome. Certain genetic
factors also may increase your risk of uric acid stones.
- Cystine stones.These stones form in people with a hereditary disorder called cystinuria that causes the kidneys to excrete too much of a specific amino acid.
Risk factors
Factors that increase your risk of developing kidney stones include:
- Family or personal history.If someone in your family has had kidney stones, you’re more likely to develop stones, too. If you’ve already had one or more kidney stones, you’re at increased risk of developing another.
Dehydration. Not drinking enough water each day can increase your risk of kidney stones. People who live in warm, dry climates and those who sweat a lot may be at higher risk than others.
- Certain diets.Eating a diet that’s high in protein, sodium (salt) and sugar may increase your risk of some types of kidney stones. This is especially true with a high-sodium diet. Too much salt in your diet increases the amount of calcium your kidneys must filter and significantly increases your risk of kidney stones.
- High body mass index (BMI), large waist size and weight gain have been linked to an increased risk of
kidney stones.
- Digestive diseases and surgery.Gastric bypass surgery, inflammatory bowel disease or chronic diarrhea can cause changes in the digestive process that affect your absorption of calcium and water, increasing the amounts of stone-forming substances in your urine.
- Other medical conditionssuch as renal tubular acidosis, cystinuria, hyperparathyroidism and repeated urinary tract infections also can increase your risk of kidney stones.
- Certain supplements and medications,such as vitamin C, dietary supplements, laxatives (when used excessively), calcium-based antacids, and certain medications used to treat
migraines or depression, can increase your risk of kidney stones.

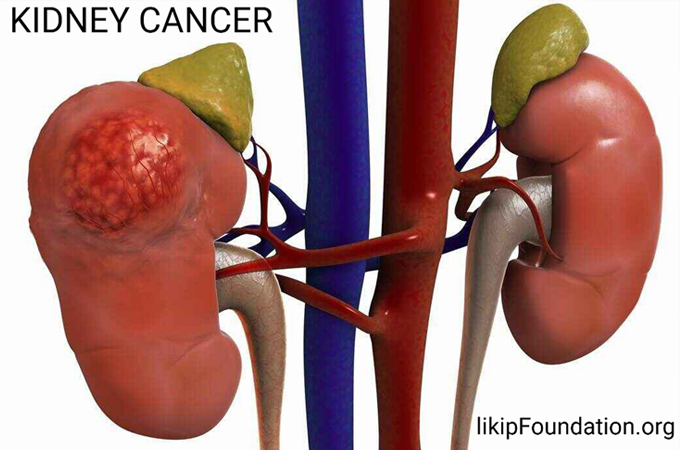
# KIDNEY CANCER
What is Kidney cancer?
Kidney cancer is cancer that begins in the kidneys
It affects twice as many men as women and is most common in middle-aged and older people, although there is an uncommon form (Wilms’ tumour, also known as nephroblastoma) that affects very young children.
Causes
kidney cancer begins when some kidney cells develop changes (mutations) in their
DNA. A cell’s DNA contains the instructions that tell a cell what to do. The changes tell the cells to grow and divide rapidly. The accumulating abnormal cells form a tumor that can extend beyond the kidney. Some cells can break off and spread (metastasize) to distant parts of the body.
Symptoms
Kidney cancer usually doesn’t have signs or symptoms in its early stages. In time, signs and symptoms may develop, including:
- Blood in your urine, which may appear pink, red or cola colored
- Pain in your back or side that doesn’t go away
- Loss of appetite
- Unexplained weight loss
- Tiredness
- Fever
Risk factors
Factors that can increase the risk of kidney cancer include:
- Older age.Your risk of kidney cancer increases as you age.
Smoking. Smokers have a greater risk of kidney cancer than nonsmokers do. The risk decreases after you quit.
- People who are obese have a higher risk of kidney cancer than people who are considered to have a healthy weight.
- High blood pressure (hypertension).High blood pressure increases your risk of kidney cancer.
- Treatment for kidney failure.People who receive long-term dialysis to treat chronic kidney failure have a greater risk of developing kidney cancer.
- Certain inherited syndromes.People who are born with certain inherited syndromes may have an increased risk
of kidney cancer, such as those who have von Hippel-Lindau disease, Birt-Hogg-Dube syndrome, tuberous sclerosis complex, hereditary papillary renal cell carcinoma or familial renal cancer.
- Family history of kidney cancer.The risk of kidney cancer is higher if close family members have had the disease.
Prevention
Taking steps to improve your health may help reduce your risk of kidney cancer. To reduce your risk, try to:
- Quit smoking.If you smoke, quit. Many options for quitting exist, including support programs, medications and nicotine replacement products. Tell your doctor you want to quit, and discuss your options together.
- Maintain a healthy weight.Work to maintain a healthy weight. If you’re overweight or obese, reduce the number of calories you consume each day and try to be physically active most days of the week. Ask your doctor about other healthy strategies to help you lose weight.
- Control high blood pressure.Ask your doctor to check your blood pressure at your next appointment. If your blood pressure is high, you can discuss options for lowering your numbers. Lifestyle measures such as exercise, weight loss and diet changes can help. Some people may need to add medications to lower their blood pressure. Discuss your options with your doctor.
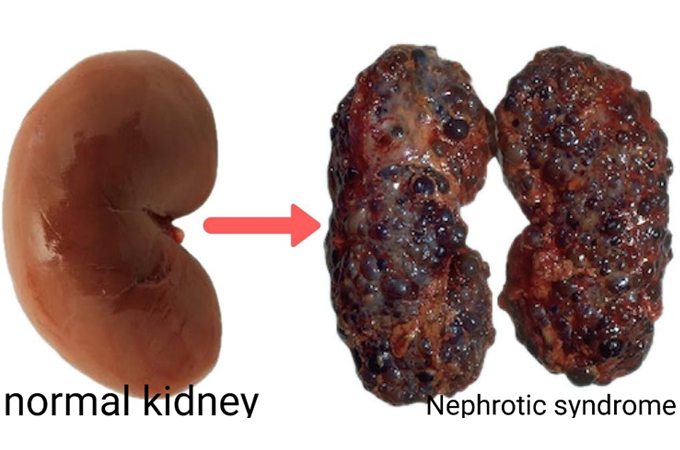
# NEPHROTIC SYNDROME
What is Nephrotic Syndrome?
Nephrotic syndrome occurs when the filters (glomeruli) in the kidney become damaged. This can happen as a result of a number of kidney diseases, such as infection, glomerulonephritis, and kidney cancer.Nephrotic syndrome is a kidney disorder that causes your body to pass too much protein in your urine.
Nephrotic syndrome is usually caused by damage to the clusters of small blood vessels in your kidneys that filter waste and excess water from your blood. The condition causes swelling, particularly in your feet and ankles, and increases the risk of other health problems.
Symptoms
Signs and symptoms of nephrotic syndrome include:
- Severe swelling (edema), particularly around your eyes and in your ankles and feet
- Foamy urine, a result of excess protein in your urine
- Weight gain due to fluid retention
- Fatigue
- Loss of appetite
Causes
Nephrotic syndrome is usually caused by damage to the clusters of tiny blood vessels (glomeruli) of your kidneys.
The glomeruli filter your blood as it passes through your kidneys, separating things your body needs from those it doesn’t. Healthy glomeruli keep blood protein (mainly albumin) — which is needed to maintain the right amount of fluid in your body — from seeping into your urine. When damaged, glomeruli allow too much blood protein to leave your body, leading to nephrotic syndrome.
Many possible causes
Many diseases and conditions can cause glomerular damage and lead to nephrotic syndrome, including:
- Diabetic kidney disease.
- Diabetes can lead to kidney damage (diabetic nephropathy) that affects the glomeruli.
- Minimal change disease.This is the most common cause of nephrotic syndrome in children. Minimal change disease results in abnormal kidney function, but when the kidney tissue is
examined under a microscope, it appears normal or nearly normal. The cause of the abnormal function typically can’t be determined.
- Focal segmental glomerulosclerosis.Characterized by scarring of some of the glomeruli, this condition can result from another disease, a genetic defect or certain medications or occur for no known reason.
- Membranous nephropathy.This kidney disorder is the result of thickening membranes within the glomeruli. The thickening is due to deposits made by the immune system. It can be associated with other medical conditions, such as lupus, hepatitis B, malaria and cancer, or it can occur for no known reason.
- Systemic lupus erythematosus.This chronic inflammatory disease can lead to serious kidney damage.
- This disorder occurs when amyloid proteins accumulate in your organs. Amyloid buildup often damages the kidneys’ filtering system.
Risk factors
Factors that can increase your risk of nephrotic syndrome include:
- Medical conditions that can damage your kidneys.Certain diseases and conditions increase your risk of developing nephrotic syndrome, such
as diabetes, lupus, amyloidosis, reflux nephropathy and other kidney diseases.
- Certain medications.Medications that might cause nephrotic syndrome include nonsteroidal anti-inflammatory drugs and drugs used to fight infections.
- Certain infections.Infections that increase the risk of nephrotic syndrome include HIV, hepatitis B, hepatitis C and malaria
Complications
Possible complications of nephrotic syndrome include:
- Blood clots.The inability of the glomeruli to filter blood properly can lead to loss of blood proteins that help prevent clotting. This increases your risk of developing a blood clot in your veins.
- High blood cholesterol and elevated blood triglycerides.
When the level of the protein albumin in your blood falls, your liver makes more albumin. At the same time, your liver releases more cholesterol and triglycerides.
- Poor nutrition.Loss of too much blood protein can result in malnutrition. This can lead to weight loss, which can be masked by edema. You may also have too few red blood cells (anemia), low blood protein levels and low levels of vitamin D.
- High blood pressure.Damage to your glomeruli and the resulting buildup of excess body fluid can raise your blood pressure.
- Acute kidney injury.If your kidneys lose their ability to filter blood due to damage to the glomeruli, waste products can build up quickly in your blood. If this happens, you might need emergency dialysis — an artificial means of removing extra fluids and waste from your blood — typically with an artificial kidney machine (dialyzer).
- Chronic kidney disease.Nephrotic syndrome can cause your kidneys to lose their function over time. If kidney function falls low enough, you might need dialysis or a kidney transplant.
- People with nephrotic syndrome have an increased risk of infections
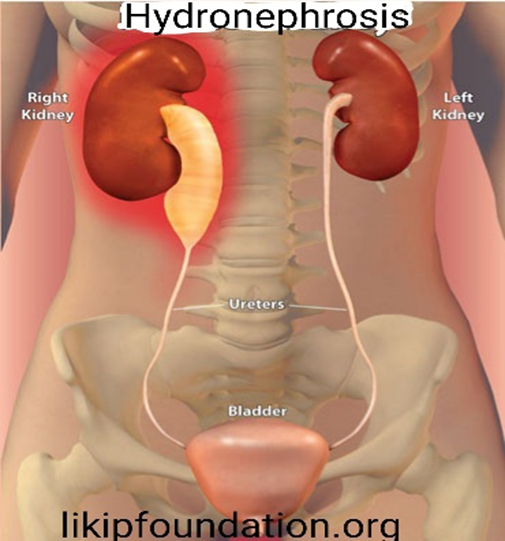
# HYDRONEPHROSIS
What is Hydronephrosis?
Hydronephrosis is the swelling of a kidney due to a build-up of urine. It happens when urine cannot drain out from the kidney to the bladder from a blockage or obstruction. Hydronephrosis can occur in one or both kidneys.
The main function of the urinary tract is to remove wastes and fluid from the body. The urinary tract has four parts: the kidneys, the ureters, the bladder and urethra. The urine is formed when the kidneys filter blood and remove excess waste materials and fluid. Urine collects into a part of the kidney called the renal pelvis. From the renal pelvis, the urine travels down a narrow tube called the ureter into the bladder. The bladder slowly fills up with urine, which empties from the body through another small tube called the urethra. Hydronephrosis occurs when there is either a blockage of the outflow of urine, or reverse flow of urine already in the bladder (called reflux) that can cause the renal pelvis to become enlarged. Hydronephrosis may or may not cause symptoms. The main symptom is pain, either in the side and back (known as flank pain), abdomen or groin. Other symptoms can include pain during urination, other problems with urination (increased urge or frequency, incomplete urination, incontinence), nausea and fever. These symptoms depend on the cause and severity of urinary blockage.
How is Hydronephrosis Caused?
Hydronephrosis is usually caused by another underlying illness or risk factor. Causes of hydronephrosis include, but are not limited to, the following illnesses or risk factors:
- Kidney stone
- Congenital blockage (a defect that is present at birth)
- Blood clot
- Scarring of tissue (from injury or previous surgery)
- Tumor or cancer (examples include bladder, cervical, colon, or prostate)
- Enlarged prostate (noncancerous)
- Pregnancy
- Urinary tract infection (or other diseases that cause inflammation of the urinary tract)
How is Hydronephrosis Treated?
Hydronephrosis is usually treated by addressing the underlying disease or cause, such as a kidney stone or infection. Some cases can be resolved without surgery. Infections can be treated with antibiotics. A kidney stone can pass through by itself or might be severe enough to require removal with surgery.
In cases of severe blockage and hydronephrosis, excess urine may need to be removed using either a catheter to drain urine from the bladder or a special tube called a nephrostomy that drains urine from the kidney. The key to treatment is to get it addressed as soon as possible in order to avoid any permanent damage to the kidneys.
Severe cases of urinary blockage and hydronephrosis can damage the kidneys and lead to kidney failure. If kidney failure occurs, treatment will be needed with either dialysis or a kidney transplant. However, most people can recover from hydronephrosis if treated promptly.
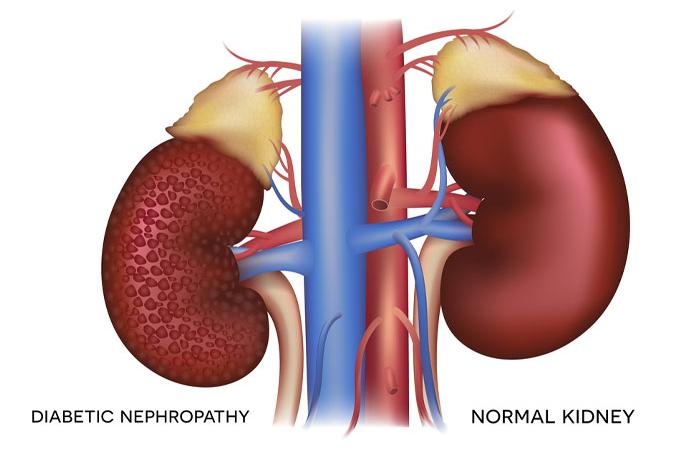
# Diabetic nephropathy
What is Diabetic nephropathy?
Diabetic nephropathy is a common complication of type 1 and type 2 diabetes.
Over time, poorly controlled diabetes can cause damage to blood vessel clusters in your kidneys that filter waste from your blood. This can lead to kidney damage and cause high blood pressure.
High blood pressure can cause further kidney damage by increasing the pressure in the delicate filtering system of the kidneys.
Risk factors
If you’re living with diabetes, factors that can increase your risk of diabetic nephropathy include:
- Uncontrolled high blood sugar (hyperglycemia)
- Uncontrolled high blood pressure (hypertension)
- Being a smoker
- High blood cholesterol
- Obesity
- A family history of diabetes and kidney disease
Complications
Complications of diabetic nephropathy may develop gradually over months or years. They may include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A rise in potassium levels in your blood (hyperkalemia)
- Heart and blood vessel disease (cardiovascular disease), which could lead to stroke
- Damage to the blood vessels of the light-sensitive tissue at the back of the eye (diabetic retinopathy)
- Reduced number of red blood cells to transport oxygen (anemia)
- Foot sores, erectile dysfunction, diarrhea and other problems related to damaged nerves and blood vessels
- Bone and mineral disorders due to the inability of the kidneys to maintain the right balance of calcium and phosphorus in the blood
- Pregnancy complications that carry risks for the mother and the developing fetus
- Irreversible damage to your kidneys (end-stage kidney disease), eventually needing either dialysis or a kidney transplant for survival
Prevention
To reduce your risk of developing diabetic nephropathy:
- Keep regular appointments for diabetes management.Keep annual appointments — or more-frequent appointments if recommended by your health care team — to monitor how well you are managing your diabetes and to screen for diabetic nephropathy and other complications.
- Treat your diabetes.With effective treatment of diabetes, you may prevent or delay diabetic nephropathy.
- Manage high blood pressure or other medical conditions.If you have high blood pressure or other conditions that increase your risk of kidney disease, work with your doctor to control them.
- Follow instructions on over-the-counter medications.Follow instructions on the packages of nonprescription pain relievers such as aspirin and nonsteroidal anti-inflammatory drugs, such as naproxen (Aleve) and ibuprofen (Advil, Motrin IB, others). For people with diabetic nephropathy, taking these types of pain relievers can lead to kidney damage.
- Maintain a healthy weight.If you’re at a healthy weight, work to maintain it by being physically active most days of the week. If you need to lose weight, talk with your doctor about weight-loss strategies, such as increasing daily physical activity and consuming fewer calories.
- Don’t smoke.Cigarette smoking can damage your kidneys and make existing kidney damage worse. If you’re a smoker, talk to your doctor about strategies for quitting smoking. Support groups, counseling and some medications can all help you to stop.
# DIABETES INSIPIDUS
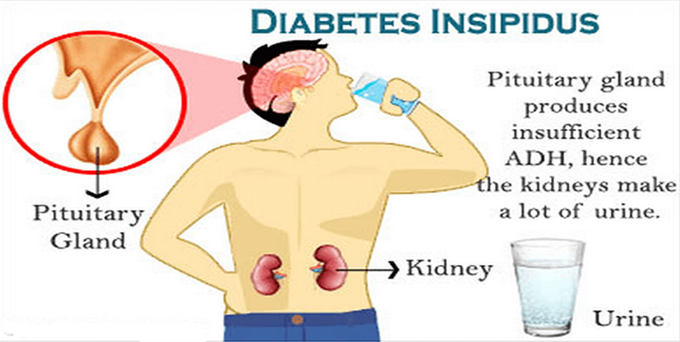
What is Diabetes insipidus?
Diabetes insipidus (die-uh-BEE-teze in-SIP-uh-dus) is an uncommon disorder that causes an imbalance of fluids in the body. This imbalance leads you to produce large amounts of urine. It also makes you very thirsty even if you have something to drink.
While the terms “diabetes insipidus” and “diabetes mellitus” sound similar, they’re not related. Diabetes mellitus — which involves high blood sugar levels and can occur as type 1 or type 2 — is common and often referred to simply as diabetes.
Symptoms
Signs and symptoms of diabetes insipidus include:
- Being extremely thirsty
- Producing large amounts of pale urine
- Frequently needing to get up to urinate during the night
- Preferring cold drinks
If your condition is serious and you drink a lot of fluids, you can produce as much as 20 quarts (about 19 liters) of urine a day. A healthy adult typically urinates an average of 1 to 2 quarts (about 1 to 2 liters) a day.
An infant or young child with diabetes insipidus may have the following signs and symptoms:
- Heavy, wet diapers
- Bed-wetting
- Trouble sleeping
- Fever
- Vomiting
- Constipation
- Delayed growth
- Weight loss
Causes
Diabetes insipidus occurs when your body can’t properly balance the body’s fluid levels. Your kidneys filter the fluid portion of your blood to remove waste products. The majority of the fluid is returned to the bloodstream while the waste and a smaller amount of fluid make up urine. Urine is excreted from your body after being temporarily stored in your bladder. A hormone called anti-diuretic hormone (ADH), or vasopressin, is needed for the fluid that’s filtered by the kidneys to go back into the bloodstream. ADH is made in a part of the brain called the hypothalamus and stored in the pituitary gland, a small
gland found in the base of the brain. Conditions that cause a deficiency of ADH or block the effect of ADH result in production of excess urine.
If you have diabetes insipidus, your body can’t properly balance fluid levels. The cause depends on the type of diabetes insipidus you have. Types include:
- Central diabetes insipidus.
Damage to the pituitary gland or hypothalamus from surgery, a tumor, head injury or illness can cause central diabetes insipidus by affecting the usual production, storage and release of ADH. An inherited genetic disease also can cause this condition.
- Nephrogenic diabetes insipidus.Nephrogenic diabetes insipidus occurs when there’s a defect in the structures in your kidneys that makes your kidneys unable to properly respond to ADH. The defect may be due to an inherited (genetic) disorder or a chronic kidney disorder. Certain drugs, such as lithium or antiviral medications such as foscarnet (Foscavir), also can cause nephrogenic diabetes insipidus.
- Gestational diabetes insipidus.Gestational diabetes insipidus is rare. It occurs only during pregnancy when an enzyme made by the placenta destroys ADH in the mother.
- Primary polydipsia.Also known as dipsogenic diabetes insipidus, this condition can cause production of large amounts of diluted urine from drinking excessive amounts of fluids.
Primary polydipsia can be caused by damage to the thirst-regulating mechanism in the hypothalamus. The condition has also been linked to mental illness, such as schizophrenia.
Sometimes, there’s no obvious cause of diabetes insipidus. However, in some people, the disorder may be the result of an autoimmune reaction that causes the immune system to damage the cells that make vasopressin.
Risk factors
Nephrogenic diabetes insipidus that’s present at or shortly after birth usually has an inherited (genetic) cause that permanently changes the kidneys’ ability to concentrate urine. Nephrogenic diabetes insipidus usually affects males, though women can pass the gene on to their children.
Complications
Dehydration
Diabetes insipidus may lead to dehydration. Dehydration can cause:
- Dry mouth
- Changes in skin elasticity
- Thirst
- Fatigue
Electrolyte imbalance
Diabetes insipidus can cause an imbalance in minerals in your blood, such as sodium and potassium (electrolytes), that maintain the fluid balance in your body. Symptoms of an electrolyte imbalance may include:
- Weakness
- Nausea
- Vomiting
- Loss of appetite
- Muscle cramps
- Confusion
- Treatment
There’s no cure for diabetes insipidus. But treatments can relieve your thirst and decrease your urine output and prevent dehydration.
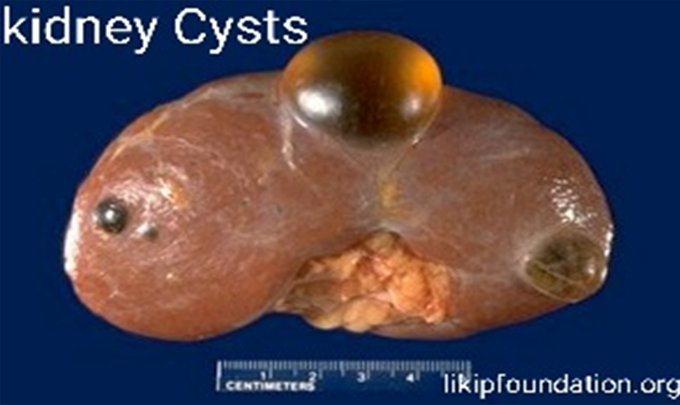
# KIDNEY CYST
What is Kidney cyst?
Kidney cysts are round pouches of fluid that form on or in the kidneys. Kidney cysts can be associated with serious disorders that may impair kidney function. But more commonly, kidney cysts are a type called simple kidney cysts — noncancerous cysts that rarely cause complications
It’s not clear what causes simple kidney cysts. Typically, only one cyst occurs on the surface of a kidney, but multiple cysts can affect one or both kidneys. However, simple kidney cysts aren’t the same as the cysts that form with polycystic kidney disease.
Simple kidney cysts are often detected during an imaging test performed for another condition. Simple kidney cysts that don’t cause signs or symptoms usually don’t require treatment.
Symptoms
Simple kidney cysts typically don’t cause
signs or symptoms. If a simple kidney cyst grows large enough, symptoms may include:
- Dull pain in your back or side
- Fever
- Upper abdominal pain
Causes
It’s not clear what causes simple kidney cysts. One theory suggests that kidney cysts develop when the surface layer of the kidney weakens and forms a pouch
(diverticulum). The pouch then fills with fluid, detaches and develops into a cyst.
Risk factors
The risk of having simple kidney cysts increases as you get older, though they can occur at any age. Simple kidney cysts are more common in men.
Complications
Kidney cysts can occasionally lead to complications, including:
- An infected cyst.A kidney cyst may become infected, causing fever and pain.
- A burst cyst.A kidney cyst that bursts causes severe pain in your back or side.
- Urine obstruction.A kidney cyst that obstructs the normal flow of urine may lead to swelling of the kidney (hydronephrosis)
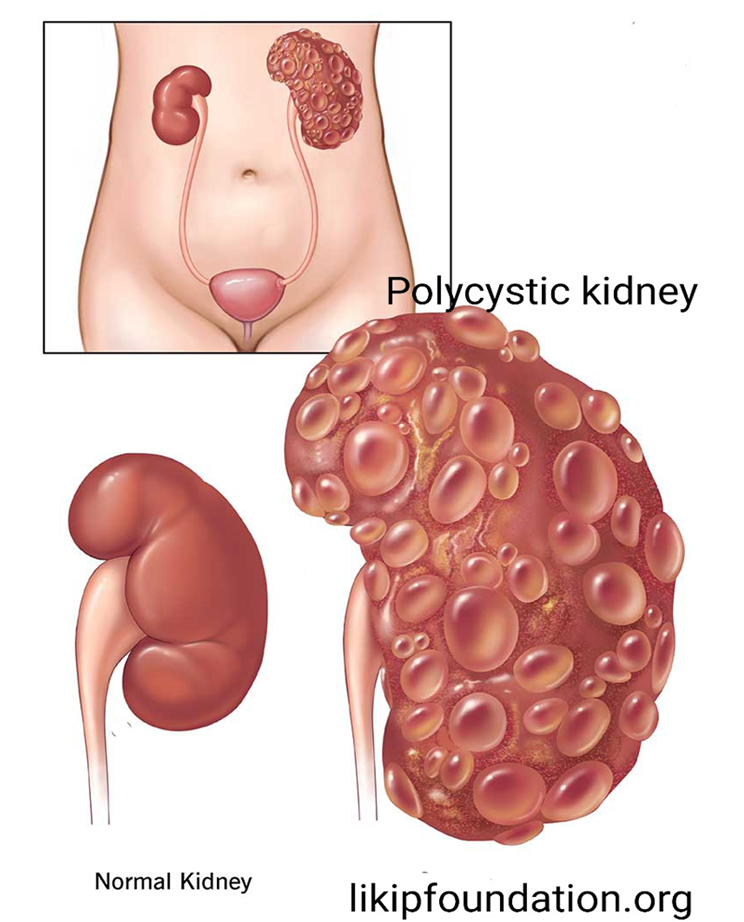
# Polycystic kidney disease (PKD)
(PKD) is an inherited disorder in which clusters of cysts develop primarily within your kidneys, causing your kidneys to enlarge and lose function over time. Cysts are noncancerous round sacs containing fluid. The cysts vary in size, and they can grow very large. Having many cysts or large cysts can damage your kidneys.
Polycystic kidney disease can also cause cysts to develop in your liver and elsewhere in your body. The disease can
cause serious complications, including high blood pressure and kidney failure.
PKD varies greatly in its severity, and some complications are preventable. Lifestyle changes and treatments might help reduce damage to your kidneys from complications.
Symptoms
Polycystic kidney disease symptoms can include:
- High blood pressure
- Back or side pain
- Blood in your urine
- A feeling of fullness in your abdomen
- Increased size of your abdomen due to enlarged kidneys
- Headaches
- Kidney stones
- Kidney failure
- Urinary tract or kidney infections
Causes
Abnormal genes cause polycystic kidney disease, which means that in most cases, the disease runs in families. Sometimes, a genetic mutation occurs on its own (spontaneous), so that neither parent has a copy of the mutated gene.
The two main types of polycystic kidney disease, caused by different genetic flaws, are:
- Autosomal dominant polycystic kidney disease (ADPKD).Signs and symptoms of ADPKD often develop between the ages of 30 and 40. In the past, this type was called adult polycystic kidney disease, but children can develop the disorder.
- Only one parent needs to have the disease for it to pass to the children. If one parent has ADPKD, each child has a 50% chance of getting the disease. This form accounts for most of the cases of polycystic kidney disease.
- Autosomal recessive polycystic kidney disease (ARPKD).This type is far less common than is ADPKD. The signs and symptoms often appear shortly after birth. Sometimes, symptoms don’t appear until later in childhood or during adolescence.
Both parents must have abnormal genes to pass on this form of the disease. If both parents carry a gene for this disorder, each child has a 25% chance of getting the disease.
Complications
Complications associated with polycystic kidney disease include:
- High blood pressure.Elevated blood pressure is a common complication of polycystic kidney disease. Untreated, high blood pressure can cause further damage to your kidneys and increase your risk of heart disease and strokes.
- Loss of kidney function.Progressive loss of kidney function is one of the most serious complications of polycystic kidney disease. Nearly half of those with the disease have kidney failure by age 60.
PKD can interfere with the ability of your kidneys to keep wastes from building to toxic levels, a condition called uremia. As the disease worsens, end-stage kidney (renal) disease may result, necessitating ongoing kidney dialysis or a transplant to prolong your life.
- Chronic pain.Pain is a common symptom for people with polycystic kidney disease. It often occurs in your side or back. The pain can also be associated with a urinary tract infection, a kidney stone or a malignancy.
- Growth of cysts in the liver.The likelihood of developing liver cysts for
someone with polycystic kidney disease increases with age. While both men and women develop cysts, women often develop larger cysts. Female hormones and multiple pregnancies might contribute to liver cyst development.
- Development of an aneurysm in the brain.A balloon-like bulge in a blood vessel (aneurysm) in your brain can cause bleeding (hemorrhage) if it ruptures. People with polycystic kidney disease have a higher risk of aneurysms. People with a family history of aneurysms seem to be at highest risk. Ask your doctor if screening is needed in your case. If screening reveals that you don’t have an aneurysm, your doctor may recommend repeating the screening
exam in a few years or after several years as a follow-up. The timing of repeat screening depends on your risk.
- Pregnancy complications.Pregnancy is successful for most women with polycystic kidney disease. In some cases, however, women may develop a life-threatening disorder called preeclampsia. Those most at risk have high blood pressure or a decline in kidney function before they become pregnant.
- Heart valve abnormalities.As many as 1 in 4 adults with polycystic kidney disease develops mitral valve prolapse. When this happens, the heart valve no longer closes properly, which allows blood to leak backward.
- Colon problems.Weaknesses and pouches or sacs in the wall of the colon (diverticulosis) may develop in people with polycystic kidney disease.
Prevention
If you have polycystic kidney disease and you’re considering having children, a genetic counselor can help you assess your risk of passing the disease to your offspring.
Keeping your kidneys as healthy as possible may help prevent some of the complications of this disease. One of the most important ways you can protect your kidneys is by managing your blood pressure.
Here are some tips for keeping your blood pressure in check:
- Take the blood pressure medications prescribed by your doctor as directed.
- Eat a low-salt diet containing plenty of fruits, vegetables and whole grains.
- Maintain a healthy weight. Ask your doctor what the right weight is for you.
- If you smoke, quit.
- Exercise regularly. Aim for at least 30 minutes of moderate physical activity most days of the week.
- Limit alcohol use.
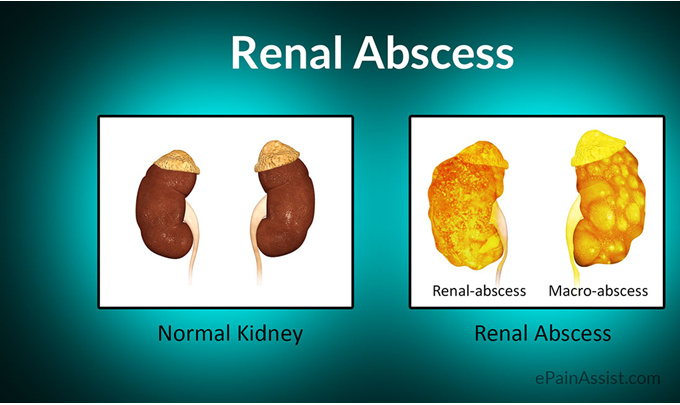
# Kidney abscess
What is kidney or renal abscess?
A renal abscess, also known as a perirenal or kidney abscess, is a pocket of pus that develops in the kidney tissue. It results from the migration of bacteria from another infection site on the body to the kidneys. Most commonly, a renal abscess if a complication of a urinary tract infection (UTI), often complicated by the existence of some blockage of urine flow.
Causes of Renal Abscess
In addition to being the result of a urinary tract infection and/or kidney stones, a renal abscess can be precipitated by one of the following:
- Skin abscess
- Intravenous drug use
- Kidney inflammation
- Kidney disease
- Reproductive or urinary tract surgery
Risk factors for a renal abscess include having diabetes, having an anatomical abnormality of the urinary tract, or having suffered a physical trauma to the kidney region.
Symptoms of a Renal Abscess
Symptoms of a renal abscess vary, but may include one or more of the following:
- Pain during urination
- Blood in the urine
- Fever and chills
- Abdominal pain
- Tenderness in the back
- Night sweats
- Weight loss
The abdominal pain experienced by patients with a renal abscess in usually felt in the side of the abdomen, and may radiate to the groin or down the leg.
Diagnosis of a Kidney Abscess
Once the doctor has taken a medical history and performed a physical examination, other tests may be administered to check for a possible kidney abscess. These diagnostic tests include the following:
- Blood culture
- Abdominal ultrasound
- Urinalysis
- Urine culture
- CT scan
Blood and urine cultures are taken to determine the type of bacteria causing the infection. Usually, the culprit is Staphylococcus aureus. Increasingly in recent years, methicillin-resistant Staphylococcus aureus (MRSA) may be to blame.
Treatment of a Kidney Abscess
A kidney abscess, once discovered, is usually treated with direct intervention. Typically, pus from the abscess is drained through a catheter inserted percutaneously (through the skin) or surgically implanted. Intravenous antibiotics are usually administered to clear the infection. If the abscess is especially large, it may have to be mechanically drained during a surgical procedure. If the patient has kidney stones, these will usually have to be removed surgically in order to eradicate the infection.
Risk of a Kidney Abscess
While a kidney abscess can almost always be treated effectively with antibiotics, there is always some small element of risk that the infection will become systemic and the patient will develop sepsis, a life-threatening condition.
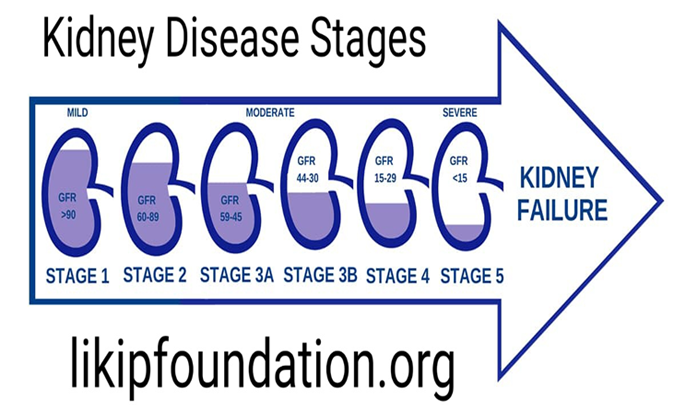
THE 5 STAGES OF CHRONIC KIDNEY DISEASE
Chronic kidney disease (CKD) is divided into five stages. The stages are based on the eGFR test result and how well your kidneys work to filter waste and extra fluid out of your blood. As the stages go up, kidney disease gets worse and your kidneys do not work as well. At each stage, it is important to take steps to slow down the damage to your kidneys.
Stages of Chronic Kidney Disease
Chronic kidney disease (CKD) is divided into five stages. The stages are based on the eGFR test result and how well your kidneys work to filter waste and extra fluid out of your blood. As the stages go up, kidney disease gets worse and your kidneys do not work as well. At each stage, it is important to take steps to slow down the damage to your kidneys.
What do the stages of chronic kidney disease (CKD) mean?
The five stages of CKD refer to how well your kidneys are working. Kidney disease can get worse in time. In the early stages (Stages 1–3), your kidneys are still able to filter waste out of your blood. In the later stages (Stages 4–5), your kidneys must work harder to filter your blood and may stop working altogether.
The goal at each stage of CKD is to take steps to slow down the damage to your kidneys and keep your kidneys working as long as possible.
How can doctors tell my stage of CKD?
To find out your stage of CKD, doctors will do tests, such as:
- eFGR tests (blood tests), which is a measure of how well your kidneys are working
- Urine (pee) tests
Stage 1 CKD: eGFR 90 or Greater
Stage 1 CKD means you have mild kidney damage and an eGFR of 90 or greater.
Most of the time, an eGFR of 90 or greater means your kidneys are healthy and working well, but you have other signs of kidney damage. Signs of kidney damage
could be protein in your urine (pee) or physical damage to your kidneys. Here are some ways to help slow down the damage to your kidneys in Stage 1 kidney disease:
- Control your blood sugar if you have diabetes
- Control your blood pressure
- Eat a healthy diet
- Do not smoke or use tobacco
- Be active 30 minutes a day, 5 days a week
- Stay at a healthy weight
- Ask your doctor if there are medicines you can take to help protect your kidneys
- Make an appointment to see a nephrologist (kidney doctor) even if you already have a general doctor
Stage 2 CKD: eGFR Between 60 and 89
Stage 2 CKD means you have mild kidney damage and an eGFR between 60 and 89.
Most of the time, an eGFR between 60 and 89 means your kidneys are healthy and working well. But if you have Stage 2 kidney disease, this means you have other signs of kidney damage even though your eGFR is normal. Signs of kidney damage could be protein in your urine (pee) or
physical damage to your kidneys. Here are some ways to help slow down the damage to your kidneys in Stage 2 kidney disease:
- Control your blood sugar if you have diabetes
- Control your blood pressure
- Eat a healthy diet
- Do not smoke or use tobacco
- Be active 30 minutes a day, 5 days a week
- Stay at a healthy weight
- Ask your doctor if there are medicines to protect your kidneys
And Make an appointment to see a nephrologist (kidney doctor) even if you already have a general doctor
Stage 3 CKD: eGFR Between 30 and 59
Stage 3 CKD means you have an eGFR between 30 and 59.
An eGFR between 30 and 59 means that there is some damage to your kidneys and they are not working as well as they should.
Stage 3 is separated into two stages:
- Stage 3a means you have an eGFR between 45 and 59
- Stage 3b means you have an eGFR between 30 and 44
Many people with Stage 3 kidney disease do not have any symptoms. But if there are symptoms, there may be:
- Swelling in your hands and feet
- Back pain
- Urinating (peeing) more or less than normal
At this stage, you are also more likely to have health complications as waste builds up in your body and your kidneys are not working well, such as:
- High blood pressure
- Anemia (a low number of red blood cells)
- Bone disease
To keep your Stage 3 kidney disease from getting worse, you can:
- Control your blood sugar if you have diabetes
- Control your blood pressure
- Do not smoke or use tobacco
- Eat a healthy diet
- Be active 30 minutes a day, 5 days a week
- Stay at a healthy weight
- Visit a nephrologist(kidney doctor), who will make a treatment plan that is right for you and tell you how often you will need to have your kidneys checked
- Meet with a dietitian, who will help you follow a healthy diet
- Ask your doctor about blood pressure medicinescalled ACE inhibitors and ARBs if you have diabetes or high blood pressure. Sometimes, these medicines can help keep kidney disease from getting worse
Stage 4 CKD: eGFR Between 15 and 29
Stage 4 CKD means you have an eGFR between 15 and 29.
An eGFR between 15 and 30 means your kidneys are moderately or severely damaged and are not working as they should. Stage 4 kidney disease should be taken very seriously – it is the last stage before kidney failure.
At Stage 4 kidney disease, many people have symptoms such as:
- Swelling in your hands and feet
- Back pain
- Urinating (peeing) more or less than normal
At Stage 4, you will likely also have health complications as waste builds up in your body and your kidneys are not working well, such as:
- High blood pressure
- Anemia (a low number of red blood cells)
- Bone disease
To keep kidney disease from getting worse at this stage, your doctor will recommend that you:
- Have regular appointments with a nephrologist(kidney doctor), who will make a treatment plan that is right for
you and tell you how often you will need to have your kidneys checked
- Meet with a dietitian, who will help you follow a healthy diet
- Take special blood pressure medicines like ACE inhibitors and ARBs if your doctor says you should. If you have diabetes or high blood pressure, sometimes these medicines can help keep kidney disease from getting worse.
At Stage 4 kidney disease, this is the time to start talking with your nephrologist about how to prepare for kidney failure. Once your kidneys have failed, you will need to start dialysis or have a kidney transplant to live.
Preparing for dialysis: Dialysis helps clean your blood when your kidneys have failed. There are several things to think about, such as the type of dialysis, how to plan your treatments and how they will affect your daily life. Learn more about hemodialysis and peritoneal dialysis.
- Preparing for a transplant:A kidney transplant is a surgery to give you a healthy kidney from someone else’s body. If you can find a living kidney donor, you may not need to start dialysis at all. It is possible to have a transplant when your kidneys are getting close to failure. Learn more about kidney transplants.
Stage 5 CKD: eGFR Less than 15
Stage 5 CKD means you have an eGFR less than 15.
An eGFR less than 15 means the kidneys are getting very close to failure or have completely failed. If your kidneys fail, waste builds up in your blood, which makes you very sick.Once your kidneys have failed, you will need to start dialysis or have a kidney transplant to live.
What is Kidney failure?
The kidneys get rid of waste products from the body. If they stop working properly, waste products can build up. This is known as kidney, or renal, failure. It can happen very quickly, over a few days, weeks or months (known as acute renal failure) or very slowly over a period of years (chronic renal failure).
When you have kidney failure, it means your kidneys are damaged. They cannot do these important jobs well enough. Having kidney failure means that:
- 85-90% of your kidney function is gone
- your kidneys don’t work well enough to keep you alive
There is no cure for kidney failure, but with treatment, it is possible to live a long life.
Having kidney failure is not a death sentence. People with kidney failure live active lives and continue to do the things they love.
What causes kidney failure?
Kidneys can become damaged from a physical injury or a disease like diabetes, high blood pressure, or other disorders. High blood pressure and diabetes are the two most common causes of kidney failure.
Kidney failure does not happen overnight. It is the end result of a gradual loss of kidney function. In fact, some people do not even know they have kidney disease until their kidneys fail. Why not? Because people with early kidney disease may not have any symptoms. Symptoms usually show up late in the progression of the
disease.
What happens when kidneys fail?
Healthy kidneys remove wastes and extra fluid from your blood. But when your kidneys fail, wastes and extra fluid can build up in your blood and make you feel sick. You may have some of the following symptoms:
- confusion
- decreased urine output
- fatigue
- difficulty concentrating
- itching
- muscle twitches and cramping
- metallic taste in your mouth
- nausea and vomiting
- loss of appetite
- seizures
- swelling in your body (edema) that starts in your ankles and legs (peripheral edema)
- shortness of breath due to fluid buildup in your lungs
- weakness (asthenia)
Once you begin treatment for kidney failure, your symptoms will improve and you will begin to feel much better.
What treatments are available for kidney failure?
There are two treatments for kidney failure — dialysis and kidney transplant. The
dialysis treatments or transplanted kidney will take over some of the work of your damaged kidneys and remove wastes and extra fluid from your body. This will make many of your symptoms better.
- Two different types of dialysis can be done — hemodialysis or peritoneal dialysis. Both remove waste products and extra fluid from your blood.
- A kidney transplant is an operation that places a healthy kidney in your body.
Eating Well on a Chronic KIDNEY Disease Diet.
What food is good for kidney patients?
When you’re living with chronic kidney disease (CKD), what you eat and drink—and how much—is important and you’ll want to start eating a kidney-friendly diet. Someone in the early stages of kidney disease may have different dietary needs than someone in the later stages. Talking to your doctor or renal dietitian will help you learn exactly what to eat and drink and why. Eating well and following a chronic kidney disease diet is key to keeping your kidneys working as long as possible.
What is a chronic kidney disease diet and how is it different?
Although a kidney-friendly diet follows many of the same basic ideas of a regular healthy diet, people living with CKD may also need to watch or limit certain foods. When your kidneys aren’t functioning at 100 percent, waste and fluid can build up in the body, causing health problems. Eating well can help your kidneys continue to function and keep you feeling your best.
People with kidney disease may need to limit their intake of:
Sodium
Potassium
Phosphorus
Protein
Fluids
In order to feel your healthiest, your individual needs may change if kidney disease progresses. Your doctor or dietitian may recommend dietary changes based on the results of your blood tests. If you already follow a certain diet for diabetes, high blood pressure, or other heart conditions, continue following those dietary recommendations as well.
Learn to read and understand nutrition labels
It’s important for people living with CKD to understand how to read nutrition labels. In addition to keeping an eye on certain nutrients, pay close attention to serving size. Be aware that the serving size listed may not match how much you actually expect to eat.
When reading nutrition labels, the % daily value (DV) tells you how much a serving of food contributes to a daily diet (based on a diet of 2,000 calories). Try sticking to the following % daily values for each serving:
Dietary fiber—more than 10% DV
Saturated fat—less than 10% DV
Trans fat—none
Sodium—less than 10% DV
Added sugars—less than 10% DV
Lighten up on protein
Your body uses protein to build and repair muscle. When you’re living with CKD, your doctor may suggest cutting back on how much protein you eat because of its effect on your kidneys. While protein is an important building block for a healthy body, it creates a waste called urea. With CKD, your body has trouble removing urea, which can make you feel tired and lose your appetite.
Choose healthier proteins
When you’re choosing proteins, it’s a good idea to avoid processed or fast foods. Instead, choose plant-based options or fresh, lean animal proteins. Watch your portion sizes and how often you eat protein-rich foods, especially if your doctor has discussed reducing your protein intake to protect your kidneys. If you’re unsure of how much protein you should eat, ask your doctor or renal dietitian for help.
Some healthy protein choices to consider include:
Plant-based proteins:
- Soy, tofu
- Beans
- Seeds
- Lentils
- Whole wheat
- Nuts
- Peanut butter
- Brown rice
- Peas
- Green beans
- Chickpeas
Animal-based proteins:
- Chicken
- Turkey
- Fish
- Shellfish
- Beef
- Pork
- Eggs
- Dairy & fresh cheese
Knowing how much protein is too much—or too little
If your kidney function is less than 25% or stage 4, you may be instructed to cut back on red meat, poultry, fish, and dairy since they contain high levels of protein. However, it’s important to understand that protein is still essential for all bodily functions, so follow your doctor or dietitian’s exact recommended protein intake.
Limit sodium and fluid intake
Healthy kidneys rid the body of excess fluid and control how much sodium is in the body. When your kidneys are not working their best, too much sodium and fluid can build up, causing swelling, high blood pressure, and stress on your heart. As such, people living with CKD may need to limit their sodium and fluid intake. Talk to your doctor or renal dietitian about how much sodium and fluid you can consume each day, and try these tips and tricks for managing your intake:
Choose fresh foods—natural foods like fresh fruits and vegetables are great low-sodium choices because they contain less sodium compared to processed and fast foods.
Read food labels closely—foods with a % Daily Value of less than 10% for sodium are good options. Watch out for “reduced sodium” or “light in sodium” options, as these can still be high in sodium or potassium.
Stick to salt-free seasonings—fresh or dried herbs, spices, and salt-free seasonings can still pack tons of flavor without the need for lots of sodium that can be hard on your kidneys.
Measure and track liquids—if your doctor has talked to you about limiting your fluids, keeping track of your daily intake is a good idea.
Why do your potassium levels matter?
The main job of the kidneys is to clean your blood of excess fluids and waste products.
When functioning normally, these fist-sized powerhouses can filter 120–150 quartsTrusted Source of blood each day, producing 1 to 2 quartsTrusted Source of urine. This helps prevent waste buildup in the body. It also helps keep electrolytes, such as sodium, phosphate, and potassium at stable levels.
People with kidney disease have diminished renal function. They’re typically unable to regulate potassium efficiently. This can cause hazardous levels of potassium to remain in the blood.
Some medications used to treat kidney disease also raise potassium, which can add to the problem.
High potassium levels usually develop slowly over weeks or months. This can lead to feelings of fatigue or nausea.
If your potassium spikes suddenly, you may experience difficulty breathing, chest pain, or heart palpitations. If you begin experiencing these symptoms, call your local emergency services. This condition, called hyperkalemia, requires immediate medical care.
How can I minimize my potassium build-up?
One of the best ways to reduce potassium buildup is to make dietary changes. To do that, you’ll need to learn which foods are high in potassium and which are low. Be sure to do your research and read the nutritional labels on your food.
Keep in mind that it isn’t just what you eat that counts, but also how much you eat. Portion control is important to the success of any kidney-friendly diet. Even a food that’s considered low in potassium can spike your levels if you eat too much of it.
Foods to add to your diet
Foods are considered low in potassium if they contain 200 milligrams (mg) or less per serving.
Some low-potassium foods include:
berries, such as strawberries and blueberries
apples
grapefruit
pineapple
cranberries and cranberry juice
cauliflower
broccoli
eggplant
green beans
white rice
white pasta
white bread
egg whites
canned tuna in water
Foods to limit or avoid
The following foods contain over 200 mg per serving.
Limit high-potassium foods such as:
bananas
avocados
raisins
prunes and prune juice
oranges and orange Juice
tomatoes, tomato juice, and tomato sauce
lentils
spinach
Brussels sprouts
split peas
potatoes (regular and sweet)
pumpkin
dried apricots
milk
bran products
low-sodium cheese
nuts
beef
chicken
Although reducing intake of potassium-rich foods is important for those on potassium restricted diets, keeping total potassium intake under the limit set by your healthcare provider, which is typically 2,000 mg of potassium per day or less, is most important.
Depending on your kidney function, you may be able to include small amounts of foods higher in potassium in your diet. Consult your healthcare provider if you have questions about your potassium restriction.
TOP SECRETS TO PREVENT KIDNEY DISEASE
- Control your blood pressure
*Take Your blood pressure medicines regularly
* Monitor your blood pressure regularly And record it
*Reduce stress, have enough rest and sleep
*Reduce your intake of salt and sodium compounds
*Do not take coffee or anything containing caffeine.
*Avoid Medications and supplements that can raise your blood pressure. From pain medications to stimulants, know which drugs and supplements can affect your blood pressure.
Some prescription and over-the-counter medications, as well as supplements and other substances, can raise your blood pressure. Certain ones can also interfere with medications intended to lower your blood pressure.
Here are some medications, supplements and other substances that can increase your blood pressure. If you’re using any of these substances and are worried about the effect it could have on your blood pressure, talk to your doctor.
Certain pain and anti-inflammatory medications can cause you to retain water, creating kidney problems and increasing your blood pressure. Examples include:
Indomethacin (Indocin, Tyvorbex)
Over-the-counter drugs such as aspirin, naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others)
Piroxicam (Feldene)
Have your blood pressure checked regularly. Talk to your doctor about which pain medication is best for you. If you must continue taking a pain medication that raises your blood pressure, your doctor may recommend lifestyle changes or additional medication to control your blood pressure.
Cold medicines (decongestants)
Decongestants narrow your blood vessels, which makes it harder for blood to flow through them, increasing blood pressure. Decongestants may also make some blood pressure medications less effective. Examples of decongestants are:
Pseudoephedrine (Sudafed 12-hour)
Phenylephrine (Neo-Synephrine)
Check the label of your cold or allergy medication to see if it contains a decongestant. If you have high blood pressure, it’s best to avoid decongestants. Ask your doctor or pharmacist about over-the-counter cold products made for people who have high blood pressure.
Antidepressants
Antidepressants work by changing your body’s response to brain chemicals, including serotonin, norepinephrine and dopamine, that affect your mood. These chemicals may also cause an increase in blood pressure. Examples of antidepressants that can raise your blood pressure are:
Monoamine oxidase inhibitors
Tricyclic antidepressants
Fluoxetine (Prozac, Sarafem)
If you take antidepressants, have your blood pressure checked regularly. If your blood pressure increases or isn’t well-controlled, ask your doctor about alternatives to these medications.
Hormonal birth control
Birth control pills and other hormonal birth control devices contain hormones that may increase your blood pressure by narrowing smaller blood vessels. Nearly all birth control pills, patches and vaginal rings come with warnings that high blood pressure may be a side effect. The risk of high blood pressure is greater if you’re older than age 35, overweight or a smoker.
Not all women will have increased blood pressure from using hormonal birth control. But if you’re worried, have your blood pressure checked at least every six to 12 months.
If you already have high blood pressure, consider using a different form of birth control. While nearly all birth control pills can raise your blood pressure, your blood pressure may be less likely to increase if you use a birth control pill or device that contains a lower dose of estrogen.
Caffeine
Caffeine can cause a temporary spike in blood pressure in people who don’t use it regularly.
Caffeine blocks a hormone that keeps your blood vessels open, allowing blood to easily pass through. This may temporarily increase blood pressure. However, there isn’t enough evidence to prove that caffeine raises your blood pressure long term.
Examples of caffeine-containing medications and products include:
Caffeine pills (Vivarin, others)
Coffee
Energy drinks and other beverages
The caffeine content of coffee can vary widely, so it’s difficult to say how many cups of coffee you can drink a day.
To see if caffeine raises your blood pressure, check your blood pressure about 30 minutes after drinking a cup of coffee or another caffeinated beverage. If your blood pressure goes up by five to 10 points, you may be sensitive to the blood pressure-raising effects of caffeine.
Herbal supplements
Remember to tell your doctor about any herbal supplements you take or are thinking about taking, to find out if the supplement could raise your blood pressure or interact with blood pressure medications. Examples of herbal supplements that can affect your blood pressure or blood pressure medications include:
Arnica (Arnica montana)
Ephedra (ma-huang)
Ginseng (Panax quinquefolius and Panax ginseng)
Guarana (Paullinia cupana)
Licorice (Glycyrrhiza glabra)
Herbal supplements aren’t necessarily safe just because they’re natural. Check with your doctor before taking any herbal supplements. You may need to avoid supplements that raise your blood pressure or interfere with your blood pressure medications.
Biological therapies
Powerful drugs used in biological therapies can have side effects, including high blood pressure. Some of these drugs target specific cells, and some use your body’s own immune system to fight a variety of autoimmune diseases and cancers.
Angiogenesis inhibitors in particular and some monoclonal antibodies can cause an increase in blood pressure. Examples of these drugs include:
Bevacizumab (Avastin)
Gefitinib (Iressa)
Imatinib (Gleevec)
Pazopanib (Votrient)
Ramucirumab (Cyramza)
Immunosuppressants
These drugs are given to nearly everyone who’s had an organ transplant. Some immunosuppressants can raise your blood pressure, possibly because of the ways immunosuppressants can affect your kidneys. Examples of immunosuppressants that can increase your blood pressure include:
Cyclosporine (Neoral, Sandimmune, Gengraf)
Tacrolimus (Astagraf XL, Prograf, Envarsus XR)
Have your blood pressure checked regularly. If your blood pressure increases or isn’t well controlled, ask your doctor about alternatives to these medications. Your doctor may recommend lifestyle changes or additional medications to control your high blood pressure.
Stimulants
Stimulants, such as methylphenidate (Ritalin, Concerta, others), can cause your heart to beat faster or irregularly, raising your blood pressure.
Have your blood pressure checked regularly if you take a stimulant. If your blood pressure increases or isn’t well controlled, ask your doctor about alternatives to these medications. He or she may recommend lifestyle changes or additional medications to control your high blood pressure.
A caution on illegal drugs
Illegal drugs can raise blood pressure by narrowing the arteries that supply blood to your heart. This increases your heart rate and damages your heart muscle.
Examples of illegal drugs that can affect your heart include:
Amphetamines, including methamphetamine
Anabolic steroids
Cocaine
MDMA
If you’re using illegal drugs, it’s important to stop. Ask your doctor for information on counseling or drug treatment programs
- Control your blood sugar
*Take your blood sugar medicines regularly
*Monitor your blood sugar regularly and record it
*Quit alcohol and late night Eating Eat your dinner latest by 4 pm.
*Practice regular exercise
- Avoid sugar excessive Carbohydrate diet.
*Avoid Medicines that Can Make Your Blood Sugar Spike.
If you have diabetes or high blood sugar, you probably know some of the things that cause your glucose (another name for blood sugar) to go up. Like a meal with too many carbohydrates, or not enough exercise. But other medicines you might take to keep yourself healthy can cause a spike, too.
Know Your Meds
Medicines you get with a prescription and some that you buy over the counter (OTC) can be a problem for people who need to control their blood sugar.
Prescription medicines that can raise your glucose include:
Steroids (also called corticosteroids). They treat diseases caused by inflammation, like rheumatoid arthritis, lupus, and allergies. Common steroids include hydrocortisone and prednisone. But steroid creams (for a rash) or inhalers (for asthma) aren’t a problem.
Drugs that treat anxiety, ADHD, depression, and other mental health problems. These can include clozapine, olanzapine, quetiapine, and risperidone.
Birth control pills
Drugs that treat high blood pressure, such as beta-blockers and thiazide diuretics
Statins to lower cholesterol
Adrenaline for severe allergic reactions
High doses of asthma medicines, or drugs that you inject for asthma treatment
Isotretinoin for acne
Tacrolimus, which you get after an organ transplant
Some medicines that treat HIV and hepatitis C
OTC medicines that can raise your blood sugar include:
Pseudoephedrine, a decongestant in some cold and flu medicines
Cough syrup. Ask your doctor if you should take regular or sugar-free.
Niacin, a B vitamin
3.Maintain a healthy weight
Obesity can increase your risk for conditions associated with kidney failure, such as diabetes and high blood pressure.
4. Eat a heart-healthy diet
A heart-healthy diet — one low in sugar and cholesterol and high in fiber, whole grains, and fruits and vegetables — helps prevent weight gain.
5. Reduce salt intake
Eating too much salt is associated with high blood pressure.
6. Drink enough water
Dehydration reduces blood flow to your kidneys, which can damage them. Ask your doctor how much water you should drink per day.
7. Limit alcohol
Alcohol increases your blood pressure. The extra calories in it can make you gain weight, too.
8. Don’t smoke
Smoking reduces blood flow to your kidneys. It damages kidney function in people with or without kidney disease.
9. Limit over-the-counter pain medication
In high doses, nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, reduce the amount of blood flow to your kidneys, which can harm them.
10. Reduce stress
Reducing stress and anxiety can lower your blood pressure, which is good for your kidneys.
11. Exercise regularly
Exercise, such as swimming, walking, and running, can help reduce stress, manage diabetes and high blood pressure, and maintain a healthy weight.
If you think you might have kidney disease, it’s important to see your doctor for evaluation. Getting an early diagnosis and treatment can help slow the progression to kidney failure.
If you know you have kidney disease, regularly see your doctor to monitor your kidney function. While chronic kidney disease can’t be reversed, its progression can be slowed with appropriate treatment.
12. Control Your cholesterol
High cholesterol increases your risk of heart disease and kidney disease. Medications can help improve your cholesterol. But if you’d rather first make lifestyle changes to improve your cholesterol, try these healthy changes.
- Reduce saturated fats.Saturated fats, found primarily in red meat and full-fat dairy products, raise your total cholesterol. Decreasing your consumption of saturated fats can reduce your low-density lipoprotein (LDL) cholesterol — the “bad” cholesterol.
- Eliminate trans fats.Trans fats, sometimes listed on food labels as “partially hydrogenated vegetable oil,” are often used in margarines and store-bought cookies, crackers and cakes. Trans fats raise overall cholesterol levels. The Food and Drug Administration has banned the use of partially hydrogenated vegetable oils by Jan. 1, 2021.
- Eat foods rich in omega-3 fatty acids.Omega-3 fatty acids don’t affect LDL cholesterol. But they have other heart-healthy benefits, including reducing blood pressure. Foods with omega-3 fatty acids include salmon, mackerel, herring, walnuts and flaxseeds.
- Increase soluble fiber.Soluble fiber can reduce the absorption of cholesterol into your bloodstream. Soluble fiber is found in such foods as oatmeal, kidney beans, Brussels sprouts, apples and pears.
- Add whey protein.Whey protein, which is found in dairy products, may account for many of the health benefits attributed to dairy. Studies have shown that whey protein given as a supplement lowers both LDL cholesterol and total cholesterol as well as blood pressure.
13. Practice Regular Health Check up
Regular health check-ups can identify any early signs of health issues. Finding problems early means that your chances for effective treatment are increased. Many factors, such as your age, health, family history and lifestyle choices, impact on how often you need check-ups.
Early Detection Is Key
It is a good idea to visit a doctor regularly, even if you feel healthy. The purpose of these visits is to:
- check for current or emerging medical problems
- assess your risk of future medical issues
- prompt you to maintain a healthy lifestyle
- update vaccinations.
Health checks are usually incorporated into routine medical care. Your doctor will often perform these checks when you are visiting for another condition, such as a cold or another problem. Your doctor will then tell you how often you need to have a health check.
Having a health check is also a time to examine your lifestyle to see what improvements can be made. This may be something you regularly do yourself or discuss with a healthcare professional.
14. Cook Your Own Food
We all love convenience food, but one of the simplest ways to improve your health is by preparing more home-cooked meals. Here’s how to get started.
Whether you live on your own or are a busy parent, finding the time and energy to prepare home-cooked meals can seem like a daunting task. At the end of a hectic day, eating out or ordering in might feel like the quickest, easiest option. But convenience and processed food can take a significant toll on your mood and health.
Convenience food is typically high in chemical additives, hormones, sugar, salt, unhealthy fat, and calories, all of which can adversely affect your brain and outlook. It can leave you feeling tired, bloated, and irritable, and exacerbate symptoms of depression, stress, and anxiety.
Restaurants often serve more food than you should eat. Many restaurants serve portions that are two to three times larger than the recommended dietary guidelines. This encourages you to eat more than you would at home, adversely affecting your waistline, blood pressure, and risk of diabetes.
When you prepare your own meals, you have more control over the ingredients. By cooking for yourself, you can ensure that you and your family eat fresh, wholesome meals. This can help you to look and feel healthier, boost your energy, stabilize your weight and mood, and improve your sleep and resilience to stress.
Cooking at home doesn’t have to be complicated. The cornerstone of a healthy diet is to eat food that is as close as possible to the way nature made it. That means replacing processed food with real food whenever possible and eating plenty of vegetables and healthy sources of protein. It doesn’t mean you have to spend hours in the kitchen combining hundreds of different ingredients or slavishly following elaborate recipes. In fact, simple meals are often the tastiest.
Cooking at home can even take less time that eating out. There are plenty of quick, simple, and wholesome meals you can cook at home in less time than it takes to travel to a restaurant or wait for a delivery.
Cooking at home is also a great way to spend time with others—and you don’t have to be an accomplished chef. Whatever your abilities or experience as a cook, you can learn to prepare quick and healthy meals that can have real benefits for your mental and physical health.

Share this page to educate others or click on the whatsapp below to talk to our Doctor .